Indications/Uses
For the symptomatic treatment of productive cough associated with airway disorders, such as acute and chronic bronchitis, bronchial asthma and bronchiectasis.
Dosage/Direction for Use
Salbutamol: Overdosage with salbutamol produces symptoms that may be expected with beta2-agonists such as tachycardia, central nervous system stimulation, tremor, hypokalemia, and hypoglycemia.
Nausea, vomiting and hyperglycemia have been reported, predominantly in children and when salbutamol overdose has been taken via the oral route.
Lactic acidosis has been reported in association with high therapeutic doses as well as overdoses of short-acting beta-agonist therapy.
Cardiac arrest and even death may occur following excessive use of salbutamol.
Discontinue salbutamol and institute appropriate symptomatic therapy in cases of salbutamol overdosage. Administration of a beta-adrenergic blocking agent may be appropriate, but use with caution in patients with a history of bronchospasm. There is no adequate evidence to support the use of dialysis in the treatment of salbutamol overdose.
Carbocisteine: Carbocisteine overdose is usually associated with stomach or intestinal discomfort. No active treatment is necessary.
Nausea, vomiting and hyperglycemia have been reported, predominantly in children and when salbutamol overdose has been taken via the oral route.
Lactic acidosis has been reported in association with high therapeutic doses as well as overdoses of short-acting beta-agonist therapy.
Cardiac arrest and even death may occur following excessive use of salbutamol.
Discontinue salbutamol and institute appropriate symptomatic therapy in cases of salbutamol overdosage. Administration of a beta-adrenergic blocking agent may be appropriate, but use with caution in patients with a history of bronchospasm. There is no adequate evidence to support the use of dialysis in the treatment of salbutamol overdose.
Carbocisteine: Carbocisteine overdose is usually associated with stomach or intestinal discomfort. No active treatment is necessary.
Overdosage
Salbutamol: Overdosage with salbutamol produces symptoms that may be expected with beta2-agonists such as tachycardia, central nervous system stimulation, tremor, hypokalemia, and hypoglycemia.
Nausea, vomiting and hyperglycemia have been reported, predominantly in children and when salbutamol overdose has been taken via the oral route.
Lactic acidosis has been reported in association with high therapeutic doses as well as overdoses of short-acting beta-agonist therapy.
Cardiac arrest and even death may occur following excessive use of salbutamol.
Discontinue salbutamol and institute appropriate symptomatic therapy in cases of salbutamol overdosage. Administration of a beta-adrenergic blocking agent may be appropriate, but use with caution in patients with a history of bronchospasm. There is no adequate evidence to support the use of dialysis in the treatment of salbutamol overdose.
Carbocisteine: Carbocisteine overdose is usually associated with stomach or intestinal discomfort. No active treatment is necessary.
Nausea, vomiting and hyperglycemia have been reported, predominantly in children and when salbutamol overdose has been taken via the oral route.
Lactic acidosis has been reported in association with high therapeutic doses as well as overdoses of short-acting beta-agonist therapy.
Cardiac arrest and even death may occur following excessive use of salbutamol.
Discontinue salbutamol and institute appropriate symptomatic therapy in cases of salbutamol overdosage. Administration of a beta-adrenergic blocking agent may be appropriate, but use with caution in patients with a history of bronchospasm. There is no adequate evidence to support the use of dialysis in the treatment of salbutamol overdose.
Carbocisteine: Carbocisteine overdose is usually associated with stomach or intestinal discomfort. No active treatment is necessary.
Administration
Should be taken with food.
Contraindications
Hypersensitivity to any ingredients in the product.
Certain maternal or fetal conditions may contraindicate tocolytic therapy (e.g., eclampsia or severe preeclampsia, intrauterine infection, intrauterine fetal death, antepartum hemorrhage, placenta previa, cord compression, or toxemia of pregnancy); salbutamol should not be used for threatened abortion.
Active stomach or intestinal ulcer.
Certain maternal or fetal conditions may contraindicate tocolytic therapy (e.g., eclampsia or severe preeclampsia, intrauterine infection, intrauterine fetal death, antepartum hemorrhage, placenta previa, cord compression, or toxemia of pregnancy); salbutamol should not be used for threatened abortion.
Active stomach or intestinal ulcer.
Special Precautions
Seek medical advice if either the usual relief is diminished or the usual duration of action is reduced. Do not increase the dose or frequency of administration.
Paradoxical bronchospasm: Paradoxical bronchospasm, a potentially life-threatening event, has been observed with salbutamol. If it occurs, discontinue use of the product immediately.
Deterioration of asthma: Asthma may deteriorate acutely over a period of hours or chronically over several days or longer. Increased use of beta2-agonists, especially daily use, is a sign of deterioration of asthma control and indicates the need to reassess treatment. Possible need for anti-inflammatory treatment (e.g., corticosteroids) should be considered.
Hypokalemia: Therapy with salbutamol and other beta2-agonists may produce decrease in plasma potassium concentration possibly through intracellular shunting resulting in cardiovascular undesirable effects. Use with caution in acute severe asthma where concomitant therapy with steroid, xanthine derivatives, or diuretics, and by hypoxia may result in hypokalemia; potassium concentrations should be monitored in severe asthma.
Metabolic Effects: As with other beta2-agonists, salbutamol can induce reversible metabolic changes (e.g., increased blood sugar levels). The diabetic patient may be unable to compensate for this; and thus, result in the development of ketoacidosis. Concomitant administration of corticosteroids can exaggerate this effect.
Coexisting Conditions: Use with caution in patients with the following conditions: Cardiovascular disorders including coronary insufficiency, cardiac arrhythmias, or hypertension: Salbutamol, like all other beta2-agonists, can produce clinically significant cardiovascular effects such as changes in pulse rate or blood pressure.
Convulsive disorders.
Hyperthyroidism.
Diabetes mellitus.
In patients who are unusually responsive to sympathomimetic amines.
Stomach or intestinal ulcer and gastrointestinal bleeding.
Paradoxical bronchospasm: Paradoxical bronchospasm, a potentially life-threatening event, has been observed with salbutamol. If it occurs, discontinue use of the product immediately.
Deterioration of asthma: Asthma may deteriorate acutely over a period of hours or chronically over several days or longer. Increased use of beta2-agonists, especially daily use, is a sign of deterioration of asthma control and indicates the need to reassess treatment. Possible need for anti-inflammatory treatment (e.g., corticosteroids) should be considered.
Hypokalemia: Therapy with salbutamol and other beta2-agonists may produce decrease in plasma potassium concentration possibly through intracellular shunting resulting in cardiovascular undesirable effects. Use with caution in acute severe asthma where concomitant therapy with steroid, xanthine derivatives, or diuretics, and by hypoxia may result in hypokalemia; potassium concentrations should be monitored in severe asthma.
Metabolic Effects: As with other beta2-agonists, salbutamol can induce reversible metabolic changes (e.g., increased blood sugar levels). The diabetic patient may be unable to compensate for this; and thus, result in the development of ketoacidosis. Concomitant administration of corticosteroids can exaggerate this effect.
Coexisting Conditions: Use with caution in patients with the following conditions: Cardiovascular disorders including coronary insufficiency, cardiac arrhythmias, or hypertension: Salbutamol, like all other beta2-agonists, can produce clinically significant cardiovascular effects such as changes in pulse rate or blood pressure.
Convulsive disorders.
Hyperthyroidism.
Diabetes mellitus.
In patients who are unusually responsive to sympathomimetic amines.
Stomach or intestinal ulcer and gastrointestinal bleeding.
Use In Pregnancy & Lactation
Salbutamol: Pregnancy: Pregnancy Category C. There have been reports of congenital anomalies (e.g., cleft palate and limb defects) in children of patients treated with salbutamol. Some of the mothers, however, were receiving various medications in the course of their pregnancies. Since there is no consistent pattern of congenital abnormality development, a relationship between the use of salbutamol and the development of congenital anomalies cannot be established. The safe use of carbocisteine during pregnancy has not been established. Therefore, this product should be used in pregnancy only if the potential benefit justifies the potential risk to the fetus.
Labor and Delivery: Since beta2-agonists may interfere with uterine contraction, salbutamol should be used in labor only if the potential benefit justifies the potential risk.
Lactation: Salbutamol may be secreted in breast milk. It is not known if carbocisteine is excreted in human milk. Therefore, do not administer to breastfeeding women unless, in the opinion of a physician, the potential benefit of the drug justifies the potential risk.
Labor and Delivery: Since beta2-agonists may interfere with uterine contraction, salbutamol should be used in labor only if the potential benefit justifies the potential risk.
Lactation: Salbutamol may be secreted in breast milk. It is not known if carbocisteine is excreted in human milk. Therefore, do not administer to breastfeeding women unless, in the opinion of a physician, the potential benefit of the drug justifies the potential risk.
Adverse Reactions
Salbutamol: Infections and infestations: Conjunctivitis.
Immune system disorders: Erythema multiforrne, hypersensitivity (anaphylaxis, angioedema, bronchospasm, collapse, hypotension, oropharyngeal edema, rash, urticaria), Stevens-Johnson syndrome.
Metabolism and nutrition disorders: Hypokalemia, increased appetite.
Psychiatric disorders: Drowsiness, hoarseness, hyperactivity, insomnia, nervousness.
Nervous system disorders: Central nervous stimulation, dizziness, headache, restlessness, tremor, vertigo.
Eye disorders: Mydriasis.
Ear and labyrinth disorders: Tinnitus.
Cardiac disorders: Angina, cardiac arrythmias (including atrial fibrillation, supraventricular tachycardia, and extrasystoles), chest discomfort, myocardial ischemia, palpitations, tachycardia.
Vascular disorders: Epistaxis, flushing, hypotension, pallor, peripheral vasodilatation.
Respiratory, thoracic and mediastinal disorders: Cough, paradoxical bronchospasm.
Gastrointestinal disorders: Dyspepsia, epigastric pain, nausea, stomach ache.
Musculoskeletal and connective tissue disorders: Feeling of muscle tension, muscle cramps.
Renal and urinary disorders: Difficulty in micturition.
General disorders and administration site conditions: Increased sweating, irritability, weakness.
Carbocisteine: Carbocisteine is generally safe.
Nausea, diarrhea, stomach discomfort, gastrointestinal bleeding and skin rashes are the most common undesirable effects.
Carbocisteine rarely causes dizziness, insomnia, headache, palpitations, mild lowering of blood glucose, dryness of mouth, abnormal heart rhythm (atrial fibrillation), and flatulence (gassiness).
Immune system disorders: Erythema multiforrne, hypersensitivity (anaphylaxis, angioedema, bronchospasm, collapse, hypotension, oropharyngeal edema, rash, urticaria), Stevens-Johnson syndrome.
Metabolism and nutrition disorders: Hypokalemia, increased appetite.
Psychiatric disorders: Drowsiness, hoarseness, hyperactivity, insomnia, nervousness.
Nervous system disorders: Central nervous stimulation, dizziness, headache, restlessness, tremor, vertigo.
Eye disorders: Mydriasis.
Ear and labyrinth disorders: Tinnitus.
Cardiac disorders: Angina, cardiac arrythmias (including atrial fibrillation, supraventricular tachycardia, and extrasystoles), chest discomfort, myocardial ischemia, palpitations, tachycardia.
Vascular disorders: Epistaxis, flushing, hypotension, pallor, peripheral vasodilatation.
Respiratory, thoracic and mediastinal disorders: Cough, paradoxical bronchospasm.
Gastrointestinal disorders: Dyspepsia, epigastric pain, nausea, stomach ache.
Musculoskeletal and connective tissue disorders: Feeling of muscle tension, muscle cramps.
Renal and urinary disorders: Difficulty in micturition.
General disorders and administration site conditions: Increased sweating, irritability, weakness.
Carbocisteine: Carbocisteine is generally safe.
Nausea, diarrhea, stomach discomfort, gastrointestinal bleeding and skin rashes are the most common undesirable effects.
Carbocisteine rarely causes dizziness, insomnia, headache, palpitations, mild lowering of blood glucose, dryness of mouth, abnormal heart rhythm (atrial fibrillation), and flatulence (gassiness).
Drug Interactions
Sympathomimetic agents: Salbutamol should not be administered concomitantly with other sympathomimetic agents or epinephrine since serious adverse cardiovascular effects may occur.
Beta-adrenergic blocking agents (e.g., propranolol): Beta-adrenergic blocking agents may inhibit the effect of beta-agonists such as salbutamol. It may also produce severe bronchospasm in asthmatic patients.
Diuretics: Administration of nonpotassium-sparing diuretics (e.g., loop or thiazide diuretics) may result in electrocardiographic changes and/or hypokalemia and can be acutely worsened by administration of beta2-agonists such as salbutamol, especially when the recommended dose of the beta2-agonist is exceeded.
Digoxin: Following administration of single-dose intravenous or oral salbutamol to healthy individuals who had received digoxin for 10 days, a 16% to 22% decrease in serum digoxin concentration was observed. Although the clinical importance of these findings for patients who are receiving inhaled salbutamol and digoxin on a chronic basis is unclear, patients receiving such concomitant therapy should have their serum digoxin concentration carefully evaluated.
Monoamine oxidase inhibitors (MAOIs) or Tricyclic antidepressants (TCAs): Salbutamol should be used with caution in patients receiving MAOIs or TCAs, or within 2 weeks of discontinuation of such agents, because the effect of salbutamol on the vascular system may be potentiated. Alternative therapy should be considered in patients taking MAOIs or TCAs.
Beta-adrenergic blocking agents (e.g., propranolol): Beta-adrenergic blocking agents may inhibit the effect of beta-agonists such as salbutamol. It may also produce severe bronchospasm in asthmatic patients.
Diuretics: Administration of nonpotassium-sparing diuretics (e.g., loop or thiazide diuretics) may result in electrocardiographic changes and/or hypokalemia and can be acutely worsened by administration of beta2-agonists such as salbutamol, especially when the recommended dose of the beta2-agonist is exceeded.
Digoxin: Following administration of single-dose intravenous or oral salbutamol to healthy individuals who had received digoxin for 10 days, a 16% to 22% decrease in serum digoxin concentration was observed. Although the clinical importance of these findings for patients who are receiving inhaled salbutamol and digoxin on a chronic basis is unclear, patients receiving such concomitant therapy should have their serum digoxin concentration carefully evaluated.
Monoamine oxidase inhibitors (MAOIs) or Tricyclic antidepressants (TCAs): Salbutamol should be used with caution in patients receiving MAOIs or TCAs, or within 2 weeks of discontinuation of such agents, because the effect of salbutamol on the vascular system may be potentiated. Alternative therapy should be considered in patients taking MAOIs or TCAs.
Storage
Store at temperatures not exceeding 25°C.
Action
Pharmacology: Pharmacodynamics: Salbutamol: Salbutamol is a selective short-acting beta2-agonist with a preferential effect on beta2-receptors found in the respiratory tract. It stimulates adenyl cyclase, the enzyme which catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3',5'-adenosine monophosphate (cAMP). cAMP mediates cellular responses such as bronchial smooth muscle relaxation resulting in bronchodilation.
Carbocisteine: Carbocisteine, a derivative of acetylcysteine, is a mucoregulating agent. Its major action is thought to be on the metabolism of mucus-producing cells. The mucus produced under the influence of carbocisteine has an increased content of the less viscous sialomucin and a reduced content of the highly viscous fucomucin. Sialomucins influence the rheological properties of mucus and may also, through the inhibition of kinins, reduce or prevent bronchial inflammation.
Carbocisteine also reduces the number of exacerbations associated with chronic obstructive pulmonary disease (COPD) and inhibits the adherence of bacteria (Klebsiella pneumoniae, Pseudomonas aeruginosa and Escherichia coli) and virus to human respiratory cells.
Pharmacokinetics: Salbutamol: Salbutamol is readily absorbed from the gastrointestinal tract after oral administration. Bronchodilation begins within 30 minutes after oral administration of salbutamol, peaks in 2 to 3 hours, and persists 4 to 6 hours. Plasma protein binding is around 10%.
Salbutamol undergoes first-pass metabolism in the liver, being converted to salbutamol 4'-O-sulfate. The plasma half-life of salbutamol has been estimated to range from 4 to 6 hours. Salbutamol is rapidly excreted, mainly in the urine, as metabolites and unchanged drug; a smaller proportion is excreted in the feces. Majority of a salbutamol dose given orally is excreted within 72 hours.
Carbocisteine: Carbocisteine is rapidly and well absorbed from the gastrointestinal tract. Peak serum concentration of 13.38 mg/L was achieved 1 to 2 hours after administration of 1.5 g carbocisteine. Plasma half-life was estimated to be 1.33 hours. Carbocisteine penetrates well into lung tissues and respiratory mucus, suggesting local action. Carbocisteine undergoes acetylation, decarboxylation and sulfoxidation. Most of the drug is excreted unchanged in the urine.
Carbocisteine: Carbocisteine, a derivative of acetylcysteine, is a mucoregulating agent. Its major action is thought to be on the metabolism of mucus-producing cells. The mucus produced under the influence of carbocisteine has an increased content of the less viscous sialomucin and a reduced content of the highly viscous fucomucin. Sialomucins influence the rheological properties of mucus and may also, through the inhibition of kinins, reduce or prevent bronchial inflammation.
Carbocisteine also reduces the number of exacerbations associated with chronic obstructive pulmonary disease (COPD) and inhibits the adherence of bacteria (Klebsiella pneumoniae, Pseudomonas aeruginosa and Escherichia coli) and virus to human respiratory cells.
Pharmacokinetics: Salbutamol: Salbutamol is readily absorbed from the gastrointestinal tract after oral administration. Bronchodilation begins within 30 minutes after oral administration of salbutamol, peaks in 2 to 3 hours, and persists 4 to 6 hours. Plasma protein binding is around 10%.
Salbutamol undergoes first-pass metabolism in the liver, being converted to salbutamol 4'-O-sulfate. The plasma half-life of salbutamol has been estimated to range from 4 to 6 hours. Salbutamol is rapidly excreted, mainly in the urine, as metabolites and unchanged drug; a smaller proportion is excreted in the feces. Majority of a salbutamol dose given orally is excreted within 72 hours.
Carbocisteine: Carbocisteine is rapidly and well absorbed from the gastrointestinal tract. Peak serum concentration of 13.38 mg/L was achieved 1 to 2 hours after administration of 1.5 g carbocisteine. Plasma half-life was estimated to be 1.33 hours. Carbocisteine penetrates well into lung tissues and respiratory mucus, suggesting local action. Carbocisteine undergoes acetylation, decarboxylation and sulfoxidation. Most of the drug is excreted unchanged in the urine.
MedsGo Class
Cough & Cold Preparations
Features
Dosage
2mg / 500mg / 5ml
Ingredients
- Carbocisteine
- Salbutamol
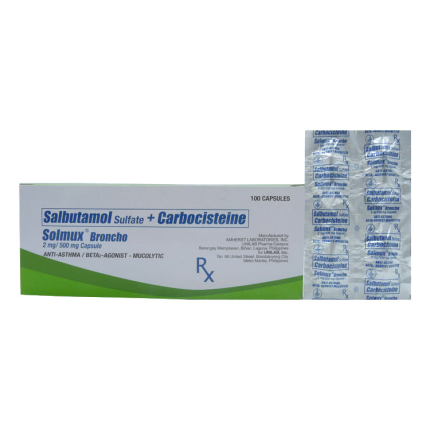
Packaging
Suspension 60ml
Generic Name
Salbutamol / Carbocisteine
Registration Number
DR-XY790
Classification
Prescription Drug (RX)
Reviews
No reviews found
Pharmacist answers to questions about SOLMUX BRONCHO Salbutamol / Carbocisteine 2mg / 500mg per 5mL Suspension 60mL
Questions