Indications/Uses
Piperacillin/tazobactam (Tazocin) is indicated for the treatment of the following systemic and/or local bacterial infections caused by gram-positive and gram-negative aerobic and anaerobic organisms susceptible to piperacillin/tazobactam or piperacillin: Adults: Lower respiratory tract infections; Urinary tract infections; Intra-abdominal infections; Skin and skin structure infections; Bacterial septicemia; Gynecological infections, including post-partum endometritis and pelvic inflammatory disease (PID); Febrile neutropenic infections. Combination treatment with an aminoglycoside is recommended; Bone and joint infections; Polymicrobial infections (gram-positive/gram-negative aerobes and anaerobes).
Children (2 years of age or older): Febrile neutropenic infections. Combination treatment with an aminoglycoside is recommended; Intra-abdominal infections.
In serious infections, empiric therapy with piperacillin/tazobactam may be initiated before susceptibility test results are available.
Note: For associated bacteremia due to extended-beta-lactamase (ESBL) producing organisms, see Pharmacology: Pharmacodynamics under Actions.
Children (2 years of age or older): Febrile neutropenic infections. Combination treatment with an aminoglycoside is recommended; Intra-abdominal infections.
In serious infections, empiric therapy with piperacillin/tazobactam may be initiated before susceptibility test results are available.
Note: For associated bacteremia due to extended-beta-lactamase (ESBL) producing organisms, see Pharmacology: Pharmacodynamics under Actions.
Dosage/Direction for Use
Piperacillin/tazobactam (Tazocin) must be given by slow intravenous infusion (e.g., over 20-30 minutes).
Duration of Therapy: The duration of therapy should be guided by the severity of the infection and the patient's clinical and bacteriological progress.
Adults and Children Aged 12 Years and Older: In general, the recommended total daily dosage is 12 g of piperacillin/1.5 g of tazobactam given in divided doses every 6 or 8 hours. Doses as high as 18 g of piperacillin/2.25 g of tazobactam per day in divided doses can be used in severe infections.
Pediatric Neutropenia: Febrile neutropenic patients in combination with an aminoglycoside: For children with normal renal function and weighing less than 50 kg, the dose should be adjusted to 80 mg of piperacillin/10 mg of tazobactam per kilogram of body weight every 6 hours, in combination with the appropriate dose of an aminoglycoside.
For children weighing over 50 kg, follow the adult dosing, in combination with the appropriate dose of an aminoglycoside.
Pediatric Intra-Abdominal Infection: For children aged 2 to 12 years, weighing up to 40 kg, and with normal renal function, the recommended dose is 100 mg piperacillin/12.5 mg tazobactam per kilogram of body weight every 8 hours.
For children aged 2 to 12 years, weighing over 40 kg, and with normal renal function, follow the adult dosing guidance. Therapy is recommended for a minimum of 5 days and a maximum of 14 days, considering that dose administration should continue at least 48 hours after the resolution of clinical signs and symptoms.
Use in Patients with Renal Impairment: In patients with renal impairment or in hemodialysis patients, intravenous dosages and administration intervals should be adjusted to the degree of renal function impairment as follows. (See Table 5.)
Duration of Therapy: The duration of therapy should be guided by the severity of the infection and the patient's clinical and bacteriological progress.
Adults and Children Aged 12 Years and Older: In general, the recommended total daily dosage is 12 g of piperacillin/1.5 g of tazobactam given in divided doses every 6 or 8 hours. Doses as high as 18 g of piperacillin/2.25 g of tazobactam per day in divided doses can be used in severe infections.
Pediatric Neutropenia: Febrile neutropenic patients in combination with an aminoglycoside: For children with normal renal function and weighing less than 50 kg, the dose should be adjusted to 80 mg of piperacillin/10 mg of tazobactam per kilogram of body weight every 6 hours, in combination with the appropriate dose of an aminoglycoside.
For children weighing over 50 kg, follow the adult dosing, in combination with the appropriate dose of an aminoglycoside.
Pediatric Intra-Abdominal Infection: For children aged 2 to 12 years, weighing up to 40 kg, and with normal renal function, the recommended dose is 100 mg piperacillin/12.5 mg tazobactam per kilogram of body weight every 8 hours.
For children aged 2 to 12 years, weighing over 40 kg, and with normal renal function, follow the adult dosing guidance. Therapy is recommended for a minimum of 5 days and a maximum of 14 days, considering that dose administration should continue at least 48 hours after the resolution of clinical signs and symptoms.
Use in Patients with Renal Impairment: In patients with renal impairment or in hemodialysis patients, intravenous dosages and administration intervals should be adjusted to the degree of renal function impairment as follows. (See Table 5.)
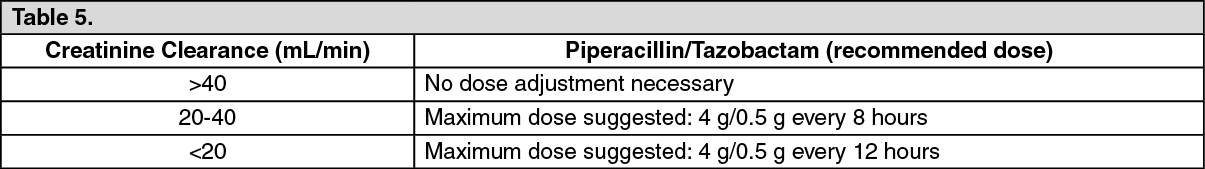
For patients on hemodialysis, one additional dose of piperacillin/tazobactam 2 g/0.25 g should be administered following each dialysis period, because hemodialysis removes 30%-50% of piperacillin in 4 hours.
Use in Patients with Hepatic Impairment: No dosage adjustment is necessary in patients with hepatic impairment.
Co-administration of Piperacillin/Tazobactam with Aminoglycosides: Due to the in vitro inactivation of the aminoglycoside by β-lactam antibiotics, piperacillin/tazobactam and the aminoglycoside are recommended for separate administration. Piperacillin/tazobactam and the aminoglycoside should be reconstituted and diluted separately when concomitant therapy with aminoglycosides is indicated (see Incompatibilities under Cautions for Usage).
In circumstances where co-administration is preferred, piperacillin/tazobactam containing EDTA supplied in vials is compatible for simultaneous co-administration via Y-site infusion only with the following aminoglycosides under the following conditions: See Table 6.
Use in Patients with Hepatic Impairment: No dosage adjustment is necessary in patients with hepatic impairment.
Co-administration of Piperacillin/Tazobactam with Aminoglycosides: Due to the in vitro inactivation of the aminoglycoside by β-lactam antibiotics, piperacillin/tazobactam and the aminoglycoside are recommended for separate administration. Piperacillin/tazobactam and the aminoglycoside should be reconstituted and diluted separately when concomitant therapy with aminoglycosides is indicated (see Incompatibilities under Cautions for Usage).
In circumstances where co-administration is preferred, piperacillin/tazobactam containing EDTA supplied in vials is compatible for simultaneous co-administration via Y-site infusion only with the following aminoglycosides under the following conditions: See Table 6.
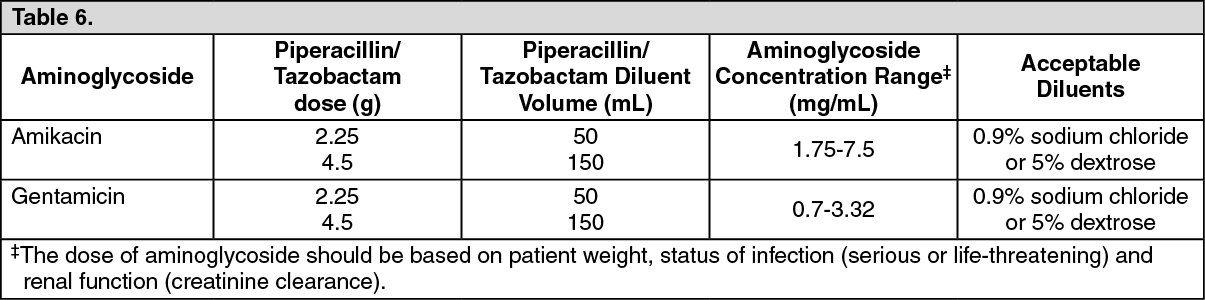
Compatibility of piperacillin/tazobactam with other aminoglycosides has not been established. Only the concentration and diluents for amikacin and gentamicin with the dosages of piperacillin/tazobactam listed in the table previously have been established as compatible for co-administration via Y-site infusion. Simultaneous co-administration via Y-site infusion in any manner other than listed previously may result in inactivation of the aminoglycoside by piperacillin/tazobactam.
Geriatric Population: Patients over 65 years are not at an increased risk of developing adverse effects solely because of age. However, dosage should be adjusted in the presence of renal insufficiency.
Geriatric Population: Patients over 65 years are not at an increased risk of developing adverse effects solely because of age. However, dosage should be adjusted in the presence of renal insufficiency.
Overdosage
Symptoms: There have been post-marketing reports of overdose with piperacillin/tazobactam. The majority of the adverse events experienced including nausea, vomiting, and diarrhea have also been reported with the usual recommended dosages. Patients may experience neuromuscular excitability or convulsions if higher than recommended doses are given intravenously (particularly in the presence of renal failure).
Treatment: Treatment should be supportive and symptomatic according to the patient's clinical presentation.
No specific antidote is known. Excessive serum concentrations of either piperacillin or tazobactam may be reduced by hemodialysis (see Pharmacology: Pharmacokinetics under Actions).
Treatment: Treatment should be supportive and symptomatic according to the patient's clinical presentation.
No specific antidote is known. Excessive serum concentrations of either piperacillin or tazobactam may be reduced by hemodialysis (see Pharmacology: Pharmacokinetics under Actions).
Contraindications
Hypersensitivity to any of the β-lactams (including penicillins and cephalosporins) or to β-lactamase inhibitors.
Special Precautions
Before initiating therapy with piperacillin/tazobactam, careful inquiry should be made concerning previous hypersensitivity reactions to penicillins, cephalosporins, and other allergens. Serious and occasionally fatal hypersensitivity (anaphylactic/anaphylactoid [including shock]) reactions have been reported in patients receiving therapy with penicillins including piperacillin/tazobactam. These reactions are more likely to occur in persons with a history of sensitivity to multiple allergens. Serious hypersensitivity reactions require discontinuation of the antibiotic, and may require administration of epinephrine and other emergency measures.
Piperacillin/tazobactam may cause severe cutaneous adverse reactions, such as Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms, and acute generalized exanthematous pustulosis (see Adverse Reactions). If patients develop a skin rash they should be monitored closely and piperacillin/tazobactam discontinued if lesions progress.
Antibiotic-induced pseudomembranous colitis may manifest as severe persistent diarrhea which may be life-threatening. The onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment.
Bleeding manifestations have occurred in some patients receiving β-lactam antibiotics. These reactions sometimes have been associated with abnormalities of coagulation tests such as clotting time, platelet aggregation and prothrombin time, and are more likely to occur in patients with renal failure (see Interactions). If bleeding manifestations occur, the antibiotic should be discontinued and appropriate therapy instituted.
This product contains 2.84 mEq (65 mg) of sodium per gram of piperacillin which may increase a patient's overall sodium intake. Hypokalemia may occur in patients with low potassium reserves or in those who are receiving concomitant medications that may lower potassium levels; periodic electrolyte determinations may be advisable in such patients.
Leukopenia and neutropenia may occur, especially during prolonged therapy. Therefore, periodic assessment of hematopoietic function should be performed.
As with treatment with other penicillins, neurological complications in the form of convulsions (seizures) may occur when high doses are administered, especially in patients with impaired renal function (see Adverse Reactions).
As with other antibiotic preparations, use of this drug may result in overgrowth of non-susceptible organisms, including fungi. Patients should be carefully monitored during therapy. If superinfection occurs, appropriate measures should be taken.
Use in Patients with Hepatic Impairment: see Dosage & Administration.
Renal Impairment: Due to its potential nephrotoxicity (see Adverse Reactions), piperacillin/tazobactam should be used with care in patients with renal impairment or in hemodialysis patients. Intravenous dosages and administration intervals should be adjusted to the degree of renal function impairment (see Use in Patients with Renal Impairment for dosage adjustments under Dosage & Administration).
In a secondary analysis using data from a large multicenter, randomized-controlled trial when glomerular filtration rate (GFR) was examined after administration of frequently used antibiotics in critically ill patients, the use of piperacillin/tazobactam was associated with a lower rate of reversible GFR improvement compared with the other antibiotics. This secondary analysis concluded that piperacillin/tazobactam was a cause of delayed renal recovery in these patients.
Combined use of piperacillin/tazobactam and vancomycin may be associated with an increased incidence of acute kidney injury (see Interactions).
Effects on Ability to Drive and Use Machines: No studies on the effect of ability to drive or use machines have been performed.
Piperacillin/tazobactam may cause severe cutaneous adverse reactions, such as Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms, and acute generalized exanthematous pustulosis (see Adverse Reactions). If patients develop a skin rash they should be monitored closely and piperacillin/tazobactam discontinued if lesions progress.
Antibiotic-induced pseudomembranous colitis may manifest as severe persistent diarrhea which may be life-threatening. The onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment.
Bleeding manifestations have occurred in some patients receiving β-lactam antibiotics. These reactions sometimes have been associated with abnormalities of coagulation tests such as clotting time, platelet aggregation and prothrombin time, and are more likely to occur in patients with renal failure (see Interactions). If bleeding manifestations occur, the antibiotic should be discontinued and appropriate therapy instituted.
This product contains 2.84 mEq (65 mg) of sodium per gram of piperacillin which may increase a patient's overall sodium intake. Hypokalemia may occur in patients with low potassium reserves or in those who are receiving concomitant medications that may lower potassium levels; periodic electrolyte determinations may be advisable in such patients.
Leukopenia and neutropenia may occur, especially during prolonged therapy. Therefore, periodic assessment of hematopoietic function should be performed.
As with treatment with other penicillins, neurological complications in the form of convulsions (seizures) may occur when high doses are administered, especially in patients with impaired renal function (see Adverse Reactions).
As with other antibiotic preparations, use of this drug may result in overgrowth of non-susceptible organisms, including fungi. Patients should be carefully monitored during therapy. If superinfection occurs, appropriate measures should be taken.
Use in Patients with Hepatic Impairment: see Dosage & Administration.
Renal Impairment: Due to its potential nephrotoxicity (see Adverse Reactions), piperacillin/tazobactam should be used with care in patients with renal impairment or in hemodialysis patients. Intravenous dosages and administration intervals should be adjusted to the degree of renal function impairment (see Use in Patients with Renal Impairment for dosage adjustments under Dosage & Administration).
In a secondary analysis using data from a large multicenter, randomized-controlled trial when glomerular filtration rate (GFR) was examined after administration of frequently used antibiotics in critically ill patients, the use of piperacillin/tazobactam was associated with a lower rate of reversible GFR improvement compared with the other antibiotics. This secondary analysis concluded that piperacillin/tazobactam was a cause of delayed renal recovery in these patients.
Combined use of piperacillin/tazobactam and vancomycin may be associated with an increased incidence of acute kidney injury (see Interactions).
Effects on Ability to Drive and Use Machines: No studies on the effect of ability to drive or use machines have been performed.
Use In Pregnancy & Lactation
Studies in animals have not shown teratogenicity with piperacillin/tazobactam combination when administered intravenously but have shown reproductive toxicity in rats at maternally toxic doses when administered intravenously or intraperitoneally. There are no adequate and well-controlled studies with the piperacillin/tazobactam combination or with piperacillin or tazobactam alone in pregnant women. Piperacillin and tazobactam cross the placenta. Pregnant women should be treated only if the expected benefit outweighs the possible risks to the pregnant woman and the fetus.
Piperacillin is excreted in low concentrations in human milk; tazobactam concentrations in human milk have not been studied. Women who are breast-feeding should be treated only if the expected benefit outweighs the possible risks to the woman and child.
Piperacillin is excreted in low concentrations in human milk; tazobactam concentrations in human milk have not been studied. Women who are breast-feeding should be treated only if the expected benefit outweighs the possible risks to the woman and child.
Adverse Reactions
See Table 7.
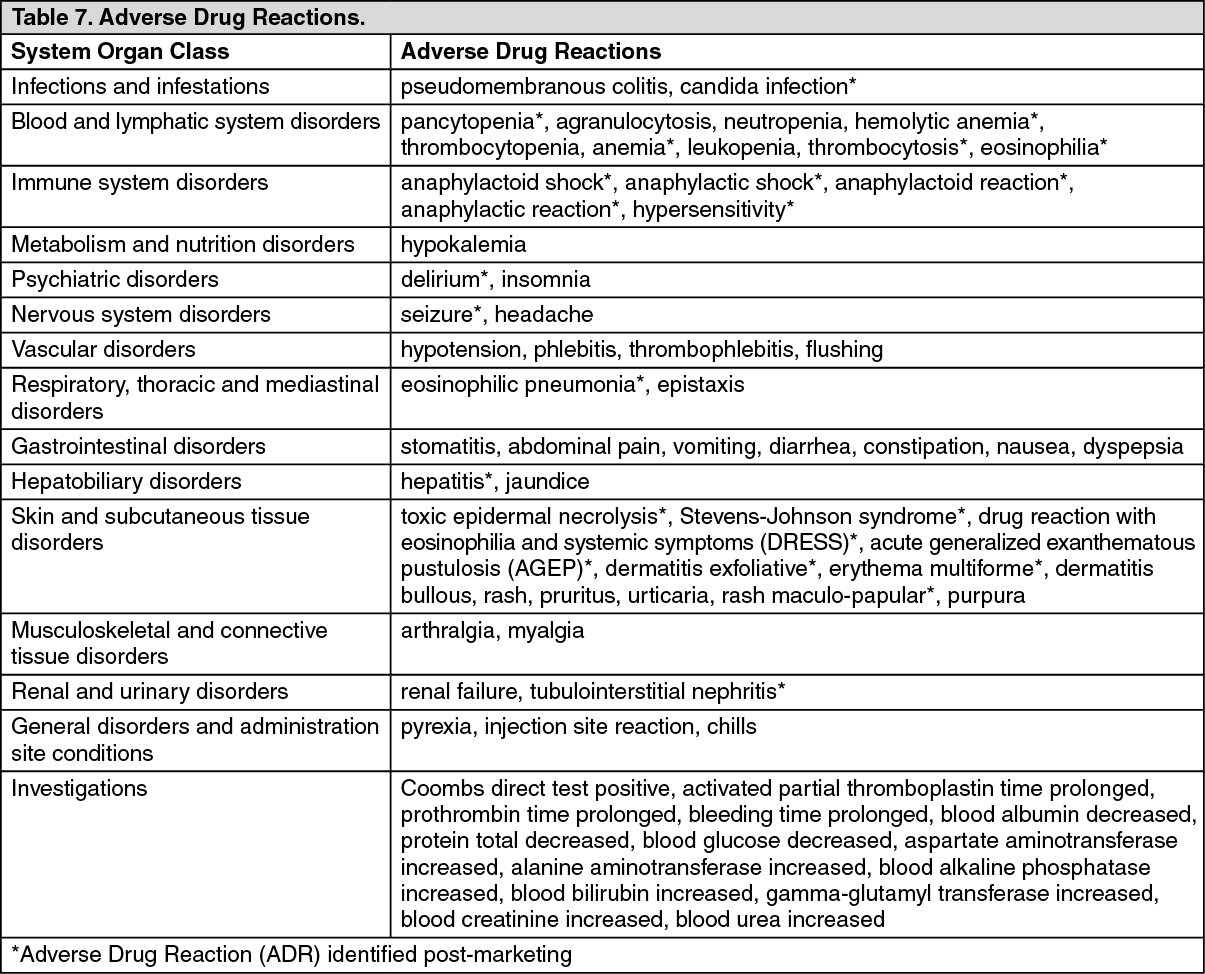
Piperacillin therapy has been associated with an increased incidence of fever and rash in cystic fibrosis patients.
Drug Interactions
Non-Depolarizing Muscle Relaxants: Piperacillin, when used concomitantly with vecuronium, has been implicated in prolonging the neuromuscular blockade of vecuronium. Due to their similar mechanism of action, it is expected that the neuromuscular blockade produced by any of the non-depolarizing muscle relaxants could be prolonged in the presence of piperacillin.
Anticoagulants: During simultaneous administration of heparin, oral anticoagulants and other drugs that may affect the blood coagulation system, including thrombocyte function, appropriate coagulation tests should be performed more frequently and monitored regularly (see Precautions).
Methotrexate: Piperacillin may reduce the excretion of methotrexate; therefore, serum levels of methotrexate should be monitored in patients to avoid drug toxicity.
Probenecid: As with other penicillins, concurrent administration of probenecid and piperacillin/tazobactam produces a longer half-life and lower renal clearance for both piperacillin and tazobactam; however, peak plasma concentrations of either drug are unaffected.
Aminoglycosides: Piperacillin, either alone or with tazobactam, did not significantly alter the pharmacokinetics of tobramycin in subjects with normal renal function and with mild or moderate renal impairment. The pharmacokinetics of piperacillin, tazobactam, and the M1 metabolite were also not significantly altered by tobramycin administration.
Vancomycin: Studies have detected an increased incidence of acute kidney injury in patients concomitantly administered piperacillin/tazobactam and vancomycin as compared to vancomycin alone (see Precautions). Some of these studies have reported that the interaction is vancomycin dose-dependent. Expert guidelines recommend intensive vancomycin dosing and maintenance of trough levels between 15 mg/L and 20 mg/L which is an increase from previously published recommendations of target trough concentrations of 5-10 mg/L. Attaining these trough concentrations often requires practitioners to prescribe vancomycin doses which exceed manufacturers' recommendations. Therefore, it is possible that in addition to the increased risk of vancomycin-induced nephrotoxicity reported with adherence to these guidelines the risk of nephrotoxicity may also increase due to an interaction with piperacillin/tazobactam.
No pharmacokinetic interactions have been noted between piperacillin/tazobactam and vancomycin.
As with other penicillins, the administration of piperacillin/tazobactam may result in a false-positive reaction for glucose in urine using a copper-reduction method. It is thus recommended that glucose tests based on enzymatic glucose oxidase reactions be used.
There have been reports of positive test results using the Bio-Rad Laboratories Platelia Aspergillus enzyme immunoassay (EIA) test in patients receiving piperacillin/tazobactam injection who were subsequently found to be free of Aspergillus infection. Cross-reactions with non-Aspergillus polysaccharides and polyfuranoses with Bio-Rad Laboratories Platelia Aspergillus EIA test have been reported.
Therefore, positive test results in patients receiving piperacillin/tazobactam should be interpreted cautiously and confirmed by other diagnostic methods.
Anticoagulants: During simultaneous administration of heparin, oral anticoagulants and other drugs that may affect the blood coagulation system, including thrombocyte function, appropriate coagulation tests should be performed more frequently and monitored regularly (see Precautions).
Methotrexate: Piperacillin may reduce the excretion of methotrexate; therefore, serum levels of methotrexate should be monitored in patients to avoid drug toxicity.
Probenecid: As with other penicillins, concurrent administration of probenecid and piperacillin/tazobactam produces a longer half-life and lower renal clearance for both piperacillin and tazobactam; however, peak plasma concentrations of either drug are unaffected.
Aminoglycosides: Piperacillin, either alone or with tazobactam, did not significantly alter the pharmacokinetics of tobramycin in subjects with normal renal function and with mild or moderate renal impairment. The pharmacokinetics of piperacillin, tazobactam, and the M1 metabolite were also not significantly altered by tobramycin administration.
Vancomycin: Studies have detected an increased incidence of acute kidney injury in patients concomitantly administered piperacillin/tazobactam and vancomycin as compared to vancomycin alone (see Precautions). Some of these studies have reported that the interaction is vancomycin dose-dependent. Expert guidelines recommend intensive vancomycin dosing and maintenance of trough levels between 15 mg/L and 20 mg/L which is an increase from previously published recommendations of target trough concentrations of 5-10 mg/L. Attaining these trough concentrations often requires practitioners to prescribe vancomycin doses which exceed manufacturers' recommendations. Therefore, it is possible that in addition to the increased risk of vancomycin-induced nephrotoxicity reported with adherence to these guidelines the risk of nephrotoxicity may also increase due to an interaction with piperacillin/tazobactam.
No pharmacokinetic interactions have been noted between piperacillin/tazobactam and vancomycin.
As with other penicillins, the administration of piperacillin/tazobactam may result in a false-positive reaction for glucose in urine using a copper-reduction method. It is thus recommended that glucose tests based on enzymatic glucose oxidase reactions be used.
There have been reports of positive test results using the Bio-Rad Laboratories Platelia Aspergillus enzyme immunoassay (EIA) test in patients receiving piperacillin/tazobactam injection who were subsequently found to be free of Aspergillus infection. Cross-reactions with non-Aspergillus polysaccharides and polyfuranoses with Bio-Rad Laboratories Platelia Aspergillus EIA test have been reported.
Therefore, positive test results in patients receiving piperacillin/tazobactam should be interpreted cautiously and confirmed by other diagnostic methods.
Caution For Usage
Incompatibilities: Solutions known to be compatible with piperacillin/tazobactam containing EDTA for reconstitution are: 0.9% Sodium chloride for injection, Sterile water for injection, Dextrose 5%, Bacteriostatic saline/parabens, Bacteriostatic water/parabens, Bacteriostatic saline/benzyl alcohol, Bacteriostatic water/benzyl alcohol.
The reconstituted solution of piperacillin/tazobactam containing EDTA may be further diluted to the desired volume (e.g., 50 mL to 150 mL) with one of the compatible solvents for intravenous use listed as follows: 0.9% Sodium chloride for injection, Sterile water for injection†, Dextrose 5%, Dextran 6% in saline, Lactated Ringer's Injection, Hartmann's solution, Ringer's acetate, Ringer's acetate/malate.
†Maximum recommended volume of sterile water for injection per dose is 50 mL.
Whenever piperacillin/tazobactam is used concurrently with another antibiotic (e.g., aminoglycosides), the drugs must be administered separately. The mixing of piperacillin/tazobactam with an aminoglycoside in vitro can result in substantial inactivation of the aminoglycoside.
The mixing of β-lactam antibiotics with aminoglycosides in vitro can result in substantial inactivation of the aminoglycoside. However, amikacin and gentamicin were determined to be compatible with piperacillin/tazobactam in vitro in certain diluents at specific concentrations (see Dosage & Administration).
Piperacillin/tazobactam should not be mixed with other drugs in a syringe or infusion bottle since compatibility has not been established.
Because of chemical instability, piperacillin/tazobactam should not be used with solutions containing only sodium bicarbonate.
Piperacillin/tazobactam should not be added to blood products or albumin hydrolysates.
Special Precautions for Disposal and Other Handling: Directions for Reconstitution and Dilution for Use: Intravenous use only: Reconstitute each vial with the volume of solvent shown in the table as follows, using one of the compatible solvents for reconstitution. Swirl until dissolved.
When swirled constantly, reconstitution generally occurs within 5 to 10 minutes. (See Table 8.)
The reconstituted solution of piperacillin/tazobactam containing EDTA may be further diluted to the desired volume (e.g., 50 mL to 150 mL) with one of the compatible solvents for intravenous use listed as follows: 0.9% Sodium chloride for injection, Sterile water for injection†, Dextrose 5%, Dextran 6% in saline, Lactated Ringer's Injection, Hartmann's solution, Ringer's acetate, Ringer's acetate/malate.
†Maximum recommended volume of sterile water for injection per dose is 50 mL.
Whenever piperacillin/tazobactam is used concurrently with another antibiotic (e.g., aminoglycosides), the drugs must be administered separately. The mixing of piperacillin/tazobactam with an aminoglycoside in vitro can result in substantial inactivation of the aminoglycoside.
The mixing of β-lactam antibiotics with aminoglycosides in vitro can result in substantial inactivation of the aminoglycoside. However, amikacin and gentamicin were determined to be compatible with piperacillin/tazobactam in vitro in certain diluents at specific concentrations (see Dosage & Administration).
Piperacillin/tazobactam should not be mixed with other drugs in a syringe or infusion bottle since compatibility has not been established.
Because of chemical instability, piperacillin/tazobactam should not be used with solutions containing only sodium bicarbonate.
Piperacillin/tazobactam should not be added to blood products or albumin hydrolysates.
Special Precautions for Disposal and Other Handling: Directions for Reconstitution and Dilution for Use: Intravenous use only: Reconstitute each vial with the volume of solvent shown in the table as follows, using one of the compatible solvents for reconstitution. Swirl until dissolved.
When swirled constantly, reconstitution generally occurs within 5 to 10 minutes. (See Table 8.)

Storage
2.25 g: Store at temperatures not exceeding 25°C.
4.5 g: Store at temperatures not exceeding 30°C.
4.5 g: Store at temperatures not exceeding 30°C.
Action
Pharmacotherapeutic Group: Antibacterials for systemic use, combinations of penicillins including β-lactamase inhibitors. ATC code: J01C R05.
Pharmacology: Pharmacodynamics: Mechanism of Action: Sterile piperacillin sodium/tazobactam sodium (Tazocin) is an injectable antibacterial combination consisting of the semisynthetic antibiotic piperacillin sodium and the β-lactamase inhibitor tazobactam sodium for intravenous administration. Thus, piperacillin/tazobactam combines the properties of a broad-spectrum antibiotic and a β-lactamase inhibitor.
Piperacillin sodium exerts bactericidal activity by inhibiting septum formation and cell wall synthesis. Piperacillin and other β-lactam antibiotics block the terminal transpeptidation step of cell wall peptidoglycan biosynthesis in susceptible bacteria by interacting with penicillin-binding proteins (PBPs), the bacterial enzymes that carry out this reaction. In vitro, piperacillin is active against a variety of gram positive and gram-negative aerobic and anaerobic bacteria.
Piperacillin has reduced activity against bacteria harboring certain β-lactamase enzymes, which chemically inactivate piperacillin and other β-lactam antibiotics. Tazobactam sodium, which has very little intrinsic antimicrobial activity, due to its low affinity for PBPs, can restore or enhance the activity of piperacillin against many of these resistant organisms. Tazobactam is a potent inhibitor of many class A β- lactamases (penicillinases, cephalosporinases and extended spectrum enzymes). It has variable activity against class A carbapenemases and class D β-lactamases. It is not active against most class C cephalosporinases and inactive against class B metallo-β-lactamases.
Two features of piperacillin/tazobactam lead to increased activity against some organisms harboring β- lactamases that, when tested as enzyme preparations, are less inhibited by tazobactam and other inhibitors: tazobactam does not induce chromosomally mediated β-lactamases at tazobactam levels achieved with the recommended dosing regimen and piperacillin is relatively refractory to the action of some β-lactamases.
Like other β-lactam antibiotics, piperacillin, with or without tazobactam, demonstrates time-dependent bactericidal activity against susceptible organisms.
Mechanism of Resistance: There are three major mechanisms of resistance to β-lactam antibiotics: changes in the target PBPs resulting in reduced affinity for the antibiotics, destruction of the antibiotics by bacterial β-lactamases, and low intracellular antibiotic levels due to reduced uptake or active efflux of the antibiotics.
In gram-positive bacteria, changes in PBPs are a major mechanism of resistance to β-lactam antibiotics, including piperacillin/tazobactam. This mechanism is responsible for methicillin resistance in staphylococci and penicillin resistance in Streptococcus pneumoniae as well as viridans group streptococci. Resistance caused by changes in PBPs also occurs to a lesser extent in fastidious gram negative species such as Haemophilus influenzae and Neisseria gonorrhoeae. Piperacillin/tazobactam is not active against strains in which resistance to β-lactam antibiotics is determined by altered PBPs. As indicated previously, there are some β- lactamases that are not inhibited by tazobactam.
MERINO Trial (bloodstream infections due to ESBL producing organisms): In a prospective, randomized non-inferiority clinical trial, definitive (i.e., based on susceptibility confirmed in-vitro) treatment with piperacillin/tazobactam did not meet non-inferiority in regard to 30-day mortality in the treatment of blood stream infections due to ESBL producing E. coli or Klebsiella pneumoniae in critically ill adult patients. A total of 23 of 187 patients (12.3%) randomized to piperacillin/tazobactam met the primary outcome of mortality at 30 days compared with 7 of 191 (3.7%) randomized to meropenem (risk difference, 8.6% [1-sided 97.5% CI - ∞ to 14.5%]; P = 0.90 for non-inferiority). Clinical and microbiological resolution by day 4 occurred in 121 of 177 patients (68.4%) in the piperacillin/tazobactam group compared with 138 of 185 (74.6%), randomized to meropenem (risk difference, -6.2% [95% CI, -15.5 to 3.1%]; P = 0.19). The cause of the mortality imbalance is not clear. This study was not sponsored by Pfizer.
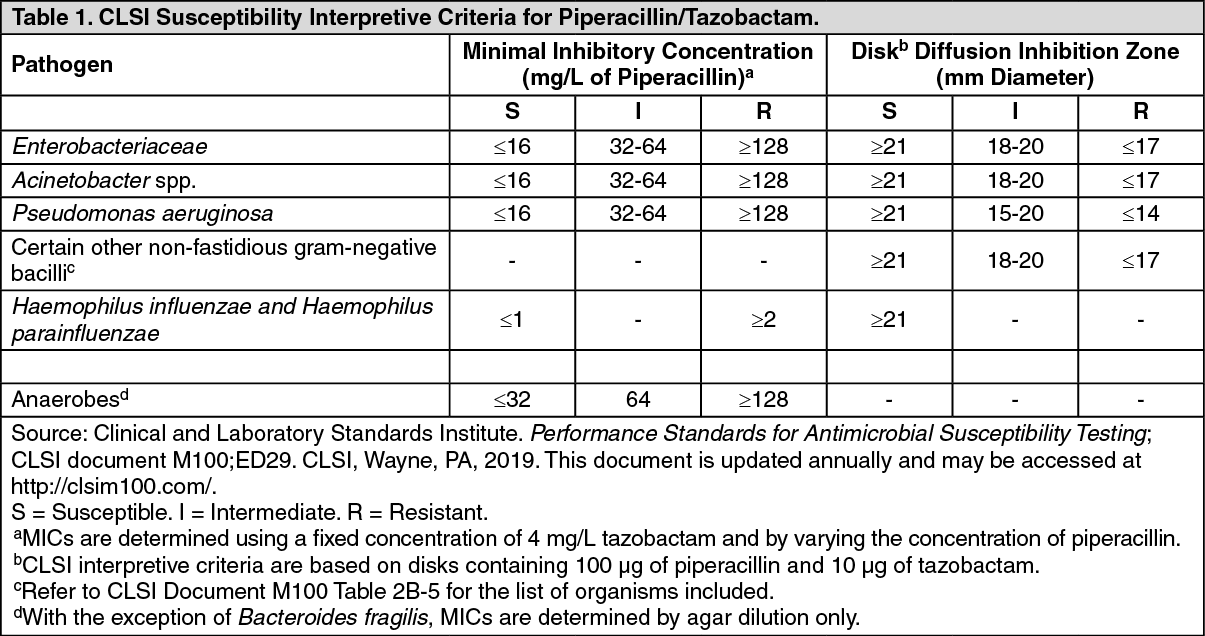
Methodology for Determining the In Vitro Susceptibility of Bacteria to Piperacillin/Tazobactam: Susceptibility testing should be conducted using standardized laboratory methods, such as those described by the Clinical and Laboratory Standards Institute (CLSI). These include dilution methods (minimal inhibitory concentration [MIC] determination) and disk susceptibility methods. Both CLSI and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) provide susceptibility interpretive criteria for some bacterial species based on these methods. It should be noted that for the disk diffusion method, CLSI and EUCAST use disks with different drug contents of piperacillin and tazobactam.
CLSI Reference Information (for markets referencing the CLSI): The CLSI interpretive criteria for susceptibility testing of piperacillin/tazobactam are listed in the following table: See Table 1.
Pharmacology: Pharmacodynamics: Mechanism of Action: Sterile piperacillin sodium/tazobactam sodium (Tazocin) is an injectable antibacterial combination consisting of the semisynthetic antibiotic piperacillin sodium and the β-lactamase inhibitor tazobactam sodium for intravenous administration. Thus, piperacillin/tazobactam combines the properties of a broad-spectrum antibiotic and a β-lactamase inhibitor.
Piperacillin sodium exerts bactericidal activity by inhibiting septum formation and cell wall synthesis. Piperacillin and other β-lactam antibiotics block the terminal transpeptidation step of cell wall peptidoglycan biosynthesis in susceptible bacteria by interacting with penicillin-binding proteins (PBPs), the bacterial enzymes that carry out this reaction. In vitro, piperacillin is active against a variety of gram positive and gram-negative aerobic and anaerobic bacteria.
Piperacillin has reduced activity against bacteria harboring certain β-lactamase enzymes, which chemically inactivate piperacillin and other β-lactam antibiotics. Tazobactam sodium, which has very little intrinsic antimicrobial activity, due to its low affinity for PBPs, can restore or enhance the activity of piperacillin against many of these resistant organisms. Tazobactam is a potent inhibitor of many class A β- lactamases (penicillinases, cephalosporinases and extended spectrum enzymes). It has variable activity against class A carbapenemases and class D β-lactamases. It is not active against most class C cephalosporinases and inactive against class B metallo-β-lactamases.
Two features of piperacillin/tazobactam lead to increased activity against some organisms harboring β- lactamases that, when tested as enzyme preparations, are less inhibited by tazobactam and other inhibitors: tazobactam does not induce chromosomally mediated β-lactamases at tazobactam levels achieved with the recommended dosing regimen and piperacillin is relatively refractory to the action of some β-lactamases.
Like other β-lactam antibiotics, piperacillin, with or without tazobactam, demonstrates time-dependent bactericidal activity against susceptible organisms.
Mechanism of Resistance: There are three major mechanisms of resistance to β-lactam antibiotics: changes in the target PBPs resulting in reduced affinity for the antibiotics, destruction of the antibiotics by bacterial β-lactamases, and low intracellular antibiotic levels due to reduced uptake or active efflux of the antibiotics.
In gram-positive bacteria, changes in PBPs are a major mechanism of resistance to β-lactam antibiotics, including piperacillin/tazobactam. This mechanism is responsible for methicillin resistance in staphylococci and penicillin resistance in Streptococcus pneumoniae as well as viridans group streptococci. Resistance caused by changes in PBPs also occurs to a lesser extent in fastidious gram negative species such as Haemophilus influenzae and Neisseria gonorrhoeae. Piperacillin/tazobactam is not active against strains in which resistance to β-lactam antibiotics is determined by altered PBPs. As indicated previously, there are some β- lactamases that are not inhibited by tazobactam.
MERINO Trial (bloodstream infections due to ESBL producing organisms): In a prospective, randomized non-inferiority clinical trial, definitive (i.e., based on susceptibility confirmed in-vitro) treatment with piperacillin/tazobactam did not meet non-inferiority in regard to 30-day mortality in the treatment of blood stream infections due to ESBL producing E. coli or Klebsiella pneumoniae in critically ill adult patients. A total of 23 of 187 patients (12.3%) randomized to piperacillin/tazobactam met the primary outcome of mortality at 30 days compared with 7 of 191 (3.7%) randomized to meropenem (risk difference, 8.6% [1-sided 97.5% CI - ∞ to 14.5%]; P = 0.90 for non-inferiority). Clinical and microbiological resolution by day 4 occurred in 121 of 177 patients (68.4%) in the piperacillin/tazobactam group compared with 138 of 185 (74.6%), randomized to meropenem (risk difference, -6.2% [95% CI, -15.5 to 3.1%]; P = 0.19). The cause of the mortality imbalance is not clear. This study was not sponsored by Pfizer.
Methodology for Determining the In Vitro Susceptibility of Bacteria to Piperacillin/Tazobactam: Susceptibility testing should be conducted using standardized laboratory methods, such as those described by the Clinical and Laboratory Standards Institute (CLSI). These include dilution methods (minimal inhibitory concentration [MIC] determination) and disk susceptibility methods. Both CLSI and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) provide susceptibility interpretive criteria for some bacterial species based on these methods. It should be noted that for the disk diffusion method, CLSI and EUCAST use disks with different drug contents of piperacillin and tazobactam.
CLSI Reference Information (for markets referencing the CLSI): The CLSI interpretive criteria for susceptibility testing of piperacillin/tazobactam are listed in the following table: See Table 1.
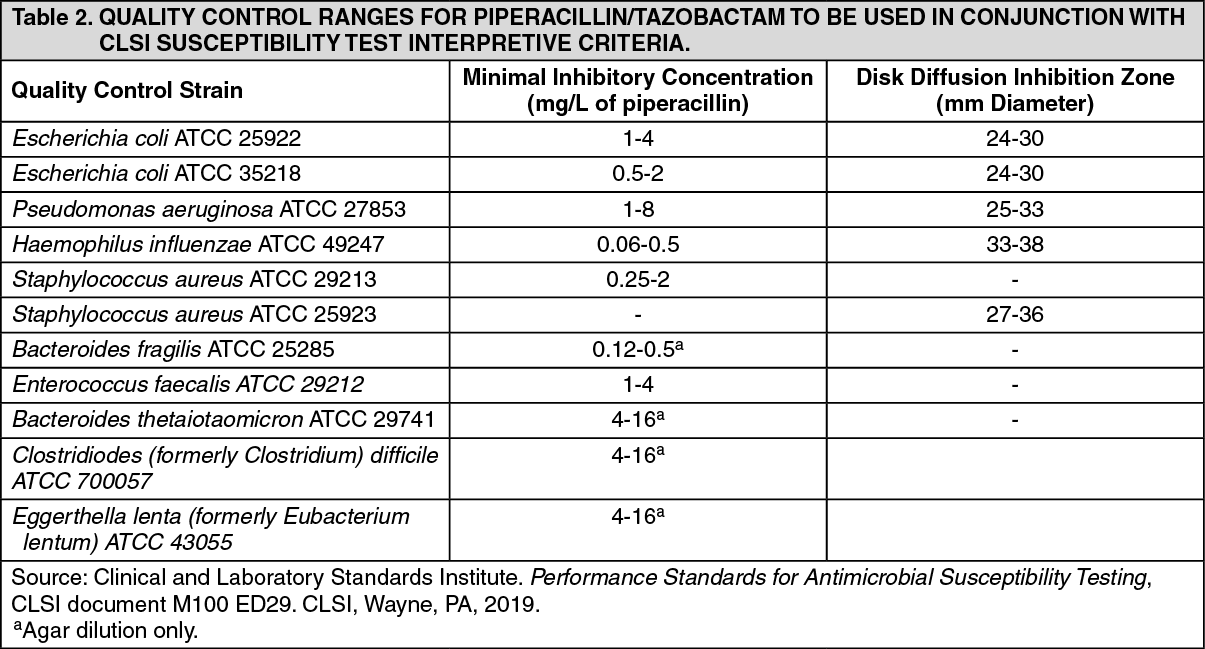
Standardized susceptibility test procedures require the use of quality control microorganisms to control the technical aspects of the test procedures. Quality control microorganisms are specific strains with intrinsic biological properties relating to resistance mechanisms and their genetic expression within the microorganism; the specific strains used for susceptibility test quality control are not clinically significant.
Organisms and quality control ranges for piperacillin/tazobactam to be utilized with CLSI methodology and susceptibility test interpretive criteria are listed in the following table: See Table 2.
Organisms and quality control ranges for piperacillin/tazobactam to be utilized with CLSI methodology and susceptibility test interpretive criteria are listed in the following table: See Table 2.
EUCAST Reference Information (for markets referencing the EUCAST): EUCAST has also established clinical breakpoints for piperacillin/tazobactam against some organisms. Like CLSI, the EUCAST MIC susceptibility criteria are based on a fixed concentration of 4 mg/L of tazobactam. However, for inhibition zone determination, the disks contain 30 μg of piperacillin and 6 μg of tazobactam. The EUCAST rationale document for piperacillin/tazobactam (Piperacillin tazobactam. Rationale for the EUCAST clinical breakpoints, version 1.0. 22nd November 2010). states that breakpoints for Pseudomonas aeruginosa apply to dosages of 4 g, 4 times daily, whereas the breakpoints for other organisms are based on 4 g, 3 times daily.y.
The EUCAST breakpoints for piperacillin/tazobactam are listed in the following table: See Table 3.
The EUCAST breakpoints for piperacillin/tazobactam are listed in the following table: See Table 3.
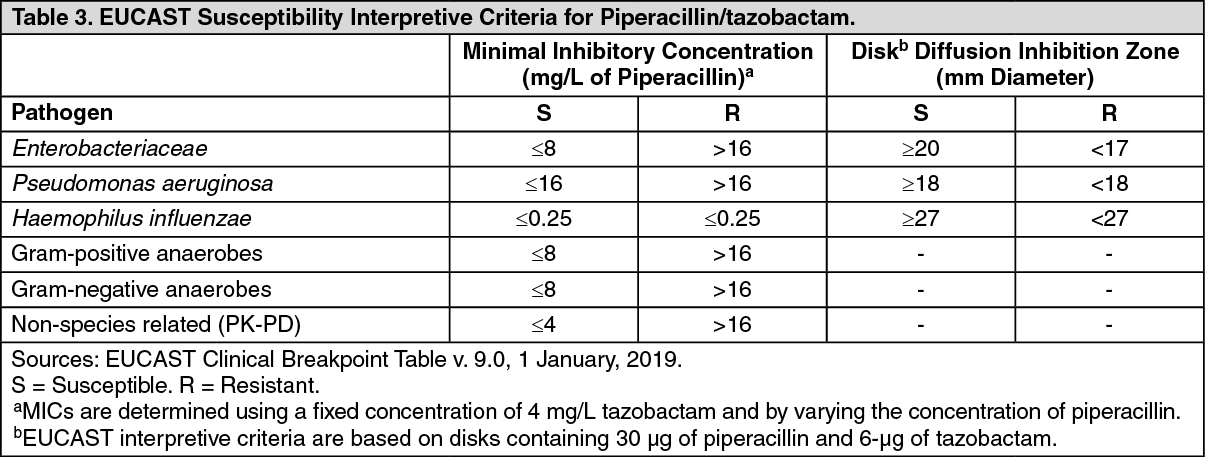
Per EUCAST, for species without piperacillin/tazobactam breakpoints, susceptibility in staphylococci is inferred from cefoxitin/oxacillin susceptibility. For groups A, B, C and G streptococci and Streptococcus pneumoniae, susceptibility is inferred from benzylpenicillin susceptibility. For other streptococci, enterococci, and β-lactamase-negative Haemophilus influenzae, susceptibility is inferred from amoxicillin-clavulanate susceptibility. There are no EUCAST breakpoints for Acinetobacter. The EUCAST rationale document for piperacillin/tazobactam states that in endocarditis caused by streptococci other than groups A, B, C and G and S. pneumoniae, national or international guidelines should be referred to.
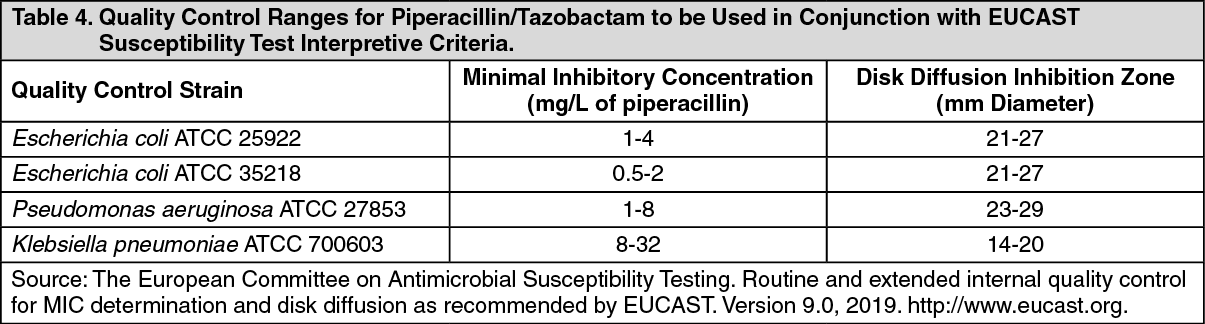
Quality control ranges for EUCAST susceptibility breakpoints are listed in the following table. (See Table 4.)
Quality control ranges for EUCAST susceptibility breakpoints are listed in the following table. (See Table 4.)
Antibacterial Spectrum (Groupings of relevant species according to piperacillin / tazobactam susceptibility): Commonly Susceptible Species: Aerobic gram-positive microorganisms: Enterococcus faecalis (ampicillin-or penicillin-susceptible isolates only), Listeria monocytogenes, Staphylococcus aureus (methicillin-susceptible isolates only), Staphylococcus spp., coagulase-negative (methicillin-susceptible isolates only), Streptococcus agalactiae (Group B streptococci)†, Streptococcus pyogenes (Group A streptococci)†.
Aerobic gram-negative microorganisms: Citrobacter koseri, Haemophilus influenzae, Moraxella catarrhalis, Proteus mirabilis.
Anaerobic gram-positive microorganisms: Clostridium spp., Eubacterium spp., Anaerobic gram-positive cocci††.
Anaerobic gram-negative microorganisms: Bacteroides fragilis group, Fusobacterium spp., Porphyromonas spp., Prevotella spp.
Species for which acquired resistance may be a problem: Aerobic gram-positive microorganisms: Enterococcus faecium, Streptococcus pneumoniae††, Viridans group streptococci††.
Aerobic gram-negative microorganisms: Acinetobacter baumannii, Citrobacter freundii, Enterobacter spp., Escherichia coli, Klebsiella pneumoniae, Morganella morganii, Proteus vulgaris, Providencia spp., Pseudomonas aeruginosa, Serratia spp.
Anaerobic gram-positive microorganisms: Clostridium perfringens.
Anaerobic gram-negative microorganisms: Bacteroides distasonis, Prevotella melaninogenica.
Inherently resistant organisms: Aerobic gram-positive microorganisms: Corynebacterium jeikeium.
Aerobic gram-negative microorganisms: Burkholderia cepacia, Legionella spp., Stenotrophomonas maltophilia.
Other microorganisms: Chlamydophila pneumoniae, Mycoplasma pneumoniae.
† Streptococci are not β-lactamase producing bacteria; resistance in these organisms is due to alterations in penicillin-binding proteins (PBPs) and, therefore, piperacillin/tazobactam-susceptible isolates are susceptible to piperacillin alone. Penicillin resistance has not been reported in S. pyogenes.
†† Including Anaerococcus, Finegoldia, Peptococcus, Peptoniphilus, and Peptostreptococcus spp. (CLSI M100 Ed. 29, 2019).
Pharmacokinetics: Distribution: Both piperacillin and tazobactam are approximately 30% bound to plasma proteins. The protein binding of either piperacillin or tazobactam is unaffected by the presence of the other compound. Protein binding of the tazobactam metabolite is negligible.
Piperacillin/tazobactam is widely distributed in tissues and body fluids including intestinal mucosa, gallbladder, lung, bile, and bone. Mean tissue concentrations are generally 50% to 100% of those in plasma.
Metabolism: Piperacillin is metabolized to a minor microbiologically active desethyl metabolite. Tazobactam is metabolized to a single metabolite that has been found to be microbiologically inactive.
Elimination: Piperacillin and tazobactam are eliminated via the kidney by glomerular filtration and tubular secretion.
Piperacillin is excreted rapidly as unchanged drug with 68% of the administered dose appearing in the urine. Tazobactam and its metabolite are eliminated primarily by renal excretion with 80% of the administered dose appearing as unchanged drug and the remainder as the single metabolite. Piperacillin, tazobactam, and desethyl piperacillin are also secreted into the bile.
Following administration of single or multiple doses of piperacillin/tazobactam to healthy subjects, the plasma half-life of piperacillin and tazobactam ranged from 0.7 to 1.2 hours and was unaffected by dose or duration of infusion. The elimination half-lives of both piperacillin and tazobactam are increased with decreasing renal clearance.
There are no significant changes in the pharmacokinetics of piperacillin due to tazobactam. Piperacillin appears to reduce the rate of elimination of tazobactam.
Special Populations: The half-lives of piperacillin and of tazobactam increase by approximately 25% and 18%, respectively, in patients with hepatic cirrhosis compared to healthy subjects.
The half-lives of piperacillin and tazobactam increase with decreasing creatinine clearance. The increase in half-life is two-fold and four-fold for piperacillin and tazobactam, respectively, at creatinine clearance below 20 mL/min compared to patients with normal renal function.
Hemodialysis removes 30% to 50% of piperacillin/tazobactam with an additional 5% of the tazobactam dose removed as the tazobactam metabolite. Peritoneal dialysis removes approximately 6% and 21% of the piperacillin and tazobactam doses, respectively, with up to 18% of the tazobactam dose removed as the tazobactam metabolite.
Toxicology: Preclinical safety data: Carcinogenicity: Carcinogenicity studies have not been conducted with piperacillin, tazobactam, or the combination.
Mutagenicity: Piperacillin/tazobactam was negative in microbial mutagenicity assays. Piperacillin/tazobactam was negative in the unscheduled DNA synthesis (UDS) test. Piperacillin/tazobactam was negative in a mammalian point mutation (Chinese hamster ovary cell hypoxanthine phosphoribosyltransferase [HPRT]) assay. Piperacillin/tazobactam was negative in a mammalian cell (BALB/c-3T3) transformation assay.
In vivo, piperacillin/tazobactam did not induce chromosomal aberrations in rats dosed intravenously.
Piperacillin was negative in microbial mutagenicity assays. There was no DNA damage in bacteria (Rec assay) exposed to piperacillin. Piperacillin was negative in the UDS test. In a mammalian point mutation (mouse lymphoma cells) assay, piperacillin was positive. Piperacillin was negative in a cell (BALB/c-3T3) transformation assay. In vivo, piperacillin did not induce chromosomal aberrations in mice dosed intravenously.
Tazobactam was negative in microbial mutagenicity assays. Tazobactam was negative in the UDS test. Tazobactam was negative in a mammalian point mutation (Chinese hamster ovary cell HPRT) assay. In another mammalian point mutation (mouse lymphoma cells) assay, tazobactam was positive. Tazobactam was negative in a cell (BALB/c-3T3) transformation assay. In an in vitro cytogenetics (Chinese hamster lung cells) assay, tazobactam was negative. In vivo, tazobactam did not induce chromosomal aberrations in rats dosed intravenously.
Reproductive Toxicity: In embryo-fetal development studies, there was no evidence of teratogenicity following intravenous administration of tazobactam or the piperacillin/tazobactam combination; however, in rats there were slight reductions in fetal body weight at maternally toxic doses.
Intraperitoneal administration of piperacillin/tazobactam was associated with slight reductions in litter size and an increased incidence of minor skeletal anomalies (delays in bone ossification) at doses that produced maternal toxicity. Peri-/post-natal development was impaired (reduced pup weights, increase in still birth, increase in pup mortality), concurrent with maternal toxicity.
Impairment of Fertility: Reproduction studies in rats revealed no evidence of impaired fertility due to tazobactam or piperacillin/tazobactam when administered intraperitoneally.
Aerobic gram-negative microorganisms: Citrobacter koseri, Haemophilus influenzae, Moraxella catarrhalis, Proteus mirabilis.
Anaerobic gram-positive microorganisms: Clostridium spp., Eubacterium spp., Anaerobic gram-positive cocci††.
Anaerobic gram-negative microorganisms: Bacteroides fragilis group, Fusobacterium spp., Porphyromonas spp., Prevotella spp.
Species for which acquired resistance may be a problem: Aerobic gram-positive microorganisms: Enterococcus faecium, Streptococcus pneumoniae††, Viridans group streptococci††.
Aerobic gram-negative microorganisms: Acinetobacter baumannii, Citrobacter freundii, Enterobacter spp., Escherichia coli, Klebsiella pneumoniae, Morganella morganii, Proteus vulgaris, Providencia spp., Pseudomonas aeruginosa, Serratia spp.
Anaerobic gram-positive microorganisms: Clostridium perfringens.
Anaerobic gram-negative microorganisms: Bacteroides distasonis, Prevotella melaninogenica.
Inherently resistant organisms: Aerobic gram-positive microorganisms: Corynebacterium jeikeium.
Aerobic gram-negative microorganisms: Burkholderia cepacia, Legionella spp., Stenotrophomonas maltophilia.
Other microorganisms: Chlamydophila pneumoniae, Mycoplasma pneumoniae.
† Streptococci are not β-lactamase producing bacteria; resistance in these organisms is due to alterations in penicillin-binding proteins (PBPs) and, therefore, piperacillin/tazobactam-susceptible isolates are susceptible to piperacillin alone. Penicillin resistance has not been reported in S. pyogenes.
†† Including Anaerococcus, Finegoldia, Peptococcus, Peptoniphilus, and Peptostreptococcus spp. (CLSI M100 Ed. 29, 2019).
Pharmacokinetics: Distribution: Both piperacillin and tazobactam are approximately 30% bound to plasma proteins. The protein binding of either piperacillin or tazobactam is unaffected by the presence of the other compound. Protein binding of the tazobactam metabolite is negligible.
Piperacillin/tazobactam is widely distributed in tissues and body fluids including intestinal mucosa, gallbladder, lung, bile, and bone. Mean tissue concentrations are generally 50% to 100% of those in plasma.
Metabolism: Piperacillin is metabolized to a minor microbiologically active desethyl metabolite. Tazobactam is metabolized to a single metabolite that has been found to be microbiologically inactive.
Elimination: Piperacillin and tazobactam are eliminated via the kidney by glomerular filtration and tubular secretion.
Piperacillin is excreted rapidly as unchanged drug with 68% of the administered dose appearing in the urine. Tazobactam and its metabolite are eliminated primarily by renal excretion with 80% of the administered dose appearing as unchanged drug and the remainder as the single metabolite. Piperacillin, tazobactam, and desethyl piperacillin are also secreted into the bile.
Following administration of single or multiple doses of piperacillin/tazobactam to healthy subjects, the plasma half-life of piperacillin and tazobactam ranged from 0.7 to 1.2 hours and was unaffected by dose or duration of infusion. The elimination half-lives of both piperacillin and tazobactam are increased with decreasing renal clearance.
There are no significant changes in the pharmacokinetics of piperacillin due to tazobactam. Piperacillin appears to reduce the rate of elimination of tazobactam.
Special Populations: The half-lives of piperacillin and of tazobactam increase by approximately 25% and 18%, respectively, in patients with hepatic cirrhosis compared to healthy subjects.
The half-lives of piperacillin and tazobactam increase with decreasing creatinine clearance. The increase in half-life is two-fold and four-fold for piperacillin and tazobactam, respectively, at creatinine clearance below 20 mL/min compared to patients with normal renal function.
Hemodialysis removes 30% to 50% of piperacillin/tazobactam with an additional 5% of the tazobactam dose removed as the tazobactam metabolite. Peritoneal dialysis removes approximately 6% and 21% of the piperacillin and tazobactam doses, respectively, with up to 18% of the tazobactam dose removed as the tazobactam metabolite.
Toxicology: Preclinical safety data: Carcinogenicity: Carcinogenicity studies have not been conducted with piperacillin, tazobactam, or the combination.
Mutagenicity: Piperacillin/tazobactam was negative in microbial mutagenicity assays. Piperacillin/tazobactam was negative in the unscheduled DNA synthesis (UDS) test. Piperacillin/tazobactam was negative in a mammalian point mutation (Chinese hamster ovary cell hypoxanthine phosphoribosyltransferase [HPRT]) assay. Piperacillin/tazobactam was negative in a mammalian cell (BALB/c-3T3) transformation assay.
In vivo, piperacillin/tazobactam did not induce chromosomal aberrations in rats dosed intravenously.
Piperacillin was negative in microbial mutagenicity assays. There was no DNA damage in bacteria (Rec assay) exposed to piperacillin. Piperacillin was negative in the UDS test. In a mammalian point mutation (mouse lymphoma cells) assay, piperacillin was positive. Piperacillin was negative in a cell (BALB/c-3T3) transformation assay. In vivo, piperacillin did not induce chromosomal aberrations in mice dosed intravenously.
Tazobactam was negative in microbial mutagenicity assays. Tazobactam was negative in the UDS test. Tazobactam was negative in a mammalian point mutation (Chinese hamster ovary cell HPRT) assay. In another mammalian point mutation (mouse lymphoma cells) assay, tazobactam was positive. Tazobactam was negative in a cell (BALB/c-3T3) transformation assay. In an in vitro cytogenetics (Chinese hamster lung cells) assay, tazobactam was negative. In vivo, tazobactam did not induce chromosomal aberrations in rats dosed intravenously.
Reproductive Toxicity: In embryo-fetal development studies, there was no evidence of teratogenicity following intravenous administration of tazobactam or the piperacillin/tazobactam combination; however, in rats there were slight reductions in fetal body weight at maternally toxic doses.
Intraperitoneal administration of piperacillin/tazobactam was associated with slight reductions in litter size and an increased incidence of minor skeletal anomalies (delays in bone ossification) at doses that produced maternal toxicity. Peri-/post-natal development was impaired (reduced pup weights, increase in still birth, increase in pup mortality), concurrent with maternal toxicity.
Impairment of Fertility: Reproduction studies in rats revealed no evidence of impaired fertility due to tazobactam or piperacillin/tazobactam when administered intraperitoneally.
MedsGo Class
Penicillins
Features
Dosage
4g / 500mg
Ingredients
- Piperacillin
- Tazobactam
Packaging
Powder for IV Injection 1's
Generic Name
Piperacillin Sodium / Tazobactam Sodium
Registration Number
DR-XY46612
Classification
Prescription Drug (RX)
Reviews
No reviews found
Product Questions
Questions