All variations
Indications/Uses
Fixcom 2: For the treatment of pulmonary and extrapulmonary tuberculosis.
Fixcom 3: For the continuation phase of pulmonary and extrapulmonary tuberculosis.
Fixcom 4: For initial or intensive phase treatment of all forms of pulmonary and extrapulmonary tuberculosis.
Fixcom 3: For the continuation phase of pulmonary and extrapulmonary tuberculosis.
Fixcom 4: For initial or intensive phase treatment of all forms of pulmonary and extrapulmonary tuberculosis.
Dosage/Direction for Use
Anti-tuberculosis short course chemotherapy recommended by World Health Organization (WHO) involves an intensive phase followed by a continuation phase for 4 months (Fixcom 2); involves an initial phase and a continuation phase (Fixcom 3); involves an initial using a combination of drugs to produce rapid killing of the tubercle bacilli (Fixcom 4).
The tablets should be taken one hour before or two hours after meals.
Fixcom 2: The dosage schedule will follow the recommended WHO TB treatment regimens. The number of tablets of fixed-dose combination tablets per patient will depend on the body weight. Hence, all patients must be weighed (using kilogram as a unit) before treatment is started. (See Table 1).
The tablets should be taken one hour before or two hours after meals.
Fixcom 2: The dosage schedule will follow the recommended WHO TB treatment regimens. The number of tablets of fixed-dose combination tablets per patient will depend on the body weight. Hence, all patients must be weighed (using kilogram as a unit) before treatment is started. (See Table 1).
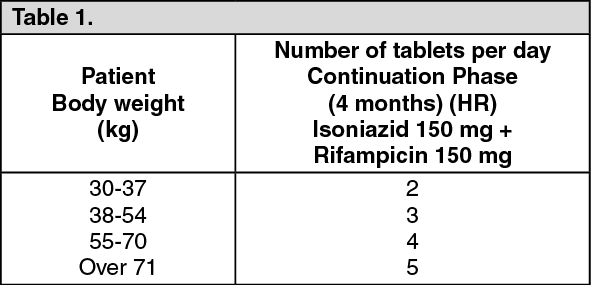
Patients <55 kg: 3 tabs/day.
Patients 55-70 kg: 4 tabs/day.
Patients >70 kg: 5 tabs/day.
Fixcom 3: The continuation phase of 4-6 months using combination drugs with the aim of elimination of any remaining organisms and thus preventing recurrence.
Fixcom 4: For the initial phase: Fixcom 4 is given for 2 months.
Ethambutol should be given in reduced dosage to patients with impaired kidney function and dosage adjustments may need to be made according to serum concentrations.
Patients 55-70 kg: 4 tabs/day.
Patients >70 kg: 5 tabs/day.
Fixcom 3: The continuation phase of 4-6 months using combination drugs with the aim of elimination of any remaining organisms and thus preventing recurrence.
Fixcom 4: For the initial phase: Fixcom 4 is given for 2 months.
Ethambutol should be given in reduced dosage to patients with impaired kidney function and dosage adjustments may need to be made according to serum concentrations.
Overdosage
Isoniazid: Symptoms of overdosage include slurred speech, metabolic acidosis, hyperglycemia, convulsions and coma; fatalities may occur.
Ethambutol: Blood concentrations of ethambutol following overdosage may be reduced by hemodialysis or peritoneal dialysis.
Ethambutol: Blood concentrations of ethambutol following overdosage may be reduced by hemodialysis or peritoneal dialysis.
Administration
Should be taken on an empty stomach: Take 1 hr before or 2 hr after meals.
Contraindications
Ethambutol: Ethambutol is generally contraindicated in patients with optic neuritis. It should be generally not be used in children <6 years and some consider that it should not be used in children <13 years nor in patients with visual defects.
Fixcom 4: Pyrazinamide: Patients with liver damage, although some consider that it can be used with care when the liver damage is not severe.
Pyrazinamide should not be given to patients with acute gout or hyperuricemia.
Fixcom 4: Pyrazinamide: Patients with liver damage, although some consider that it can be used with care when the liver damage is not severe.
Pyrazinamide should not be given to patients with acute gout or hyperuricemia.
Special Precautions
Fixcom 2: Monitoring of serum concentrations of hepatic transaminases, where possible, is useful in patients with pre-existing chronic liver disease. Patients at risk of peripheral neuropathy, as a result of malnutrition, chronic alcohol dependence or diabetes, should additionally receive pyridoxine, 10 mg daily. Where the standard of health in the community is low, this should be offered routinely.
Since isoniazid interacts with anticonvulsants used for epilepsy, it may be necessary to reduce the dosage of these drugs during treatment with isoniazid.
Rifampicin: Serious immunological reactions resulting in renal impairment, haemolysis or thrombocytopenia are on record in patients who resume taking rifampicin after a prolonged lapse of treatment. In this rare situation, it should be immediately and definitely withdrawn.
Careful monitoring of liver function is required in the elderly and in patients who are alcohol-dependent or have hepatic disease. Patients should be warned that treatment may produce reddish coloration of urine, tears, saliva and sputum and that contact lenses may be irreversibly stained.
Liver disorders: Isoniazid, rifampicin and pyrazinamide are all associated with hepatitis. Of the three drugs, rifampicin is least likely to cause hepatocellular damage, although it is associated
with cholestatic jaundice. Of the three agents, pyrazinamide is the most hepatotoxic.
Patients with the following conditions can receive the usual short-course chemotherapy regimens provided there is no clinical evidence of chronic liver disease: However, hepatotoxic reactions to antituberculosis drugs may be more common among these patients and should therefore be anticipated.
Established chronic liver disease: Patients with liver disease should not receive pyrazinamide. Isoniazid plus rifampicin plus one or two non-hepatotoxic drugs such as streptomycin and ethambutol can be used for a total treatment duration of 8 months. Alternative regimens are 9 Rifampicin/Ethambutol (RE) or Streptomycin/isoniazid Ethambutol (SHE) in the initial phase followed by Isoniazid/Ethambutol (HE) in the continuation phase. with a total treatment duration of 12 months. Recommended regimens are therefore 2SHRE/6HR. 9 RE or 2SHE/10HE.
Acute hepatitis (e.g. acute viral hepatitis): Uncommonly, a patient has TB and concurrently acute hepatitis unrelated to TB or TB treatment. Clinical judgement is necessary. In some cases, it is possible to defer TB treatment until the acute hepatitis has resolved. In other cases, when it is necessary to treat TB during acute hepatitis, the combination of Streptomycin/Ethambutol for 3 months is the safest option. If the hepatitis has resolved, the patient can then receive a continuation phase of 6 months isoniazid and rifampicin 6(HR). If the hepatitis has not resolved, Streptomycin/ethambutol should be continued for a total of 12 months.
Renal failure: Isoniazid, rifampicin and pyrazinamide are either eliminated almost entirely by biliary excretion or metabolized into non-toxic compounds. These drugs can therefore be given in normal dosage to patients with renal failure. Patients with severe renal failure should receive pyridoxine with isoniazid in order to prevent peripheral neuropathy.
Fixcom 3: Rifampicin: Liver functions should be checked before treatment with rifampicin and special care should be taken in alcoholic patients or those with preexisting liver disease who require regular monitoring during therapy. Rifampicin is contraindicated in patients with jaundice. A self-limiting hyperbilirubinemia may occur in the first 2 or 3 weeks of treatment. Alkaline phosphatase values may be raised moderately due to rifampicin's enzyme-inducing capacity. When other liver functions tests are within normal limits, hyperbilirubinemia in the 1st few weeks of moderately elevated alkaline phosphates are not indications to withdraw rifampicin. However, dose adjustment is necessary when there is other evidence of hepatic impairment and treatment should be suspended when there is evidence of more serious liver toxicity.
Blood counts should be monitored during prolonged treatment and in patients with hepatic disorders. Should thrombocytopenia or purpura occur then rifampicin should be withdrawn permanently. In patients who develop hemolytic anemia or renal failure, withdrawal of rifampicin is recommended.
Administration of rifampicin following interruption of treatment has been associated with increased risk of serious adverse effects.
Patients should be advised that rifampicin may color feces, saliva, sputum, sweat, tears, urine and other body fluids. Soft contact lenses worn by patients receiving rifampicin may become permanently stained.
Isoniazid: Isoniazid should be administered with caution to patients with convulsive disorders, a history of psychosis or hepatic or renal dysfunction. Patients who are at risk of neuropathy or pyridoxine deficiency, including those who are diabetic, alcoholic, malnourished, uremic, pregnant or HIV-infected, should receive pyridoxine usually in a dose of 10 mg daily, although some have suggested using up to 50 mg daily. If symptoms of hepatitis eg, malaise, fatigue, anorexia and nausea develop, isoniazid should be discontinued pending evaluation.
Liver function should be checked before treatment with isoniazid and special care should be taken in alcoholic patients or those with preexisting liver disease. Regular monitoring of liver function is recommended in patients with preexisting liver disease and isoniazid treatment should be suspended if serum aspartate aminotransferase concentrations are elevated to 3-5 times the normal upper limit or the bilirubin concentration rises. Periodic eye examination during isoniazid treatment have also been suggested.
Ethambutol: It should be used with great care in patients with visual defects, the elderly and in children whom evaluation changes in visual acuity may be difficult. Ocular examination is recommended before treatment with ethambutol and some consider regular examinations are necessary during treatment especially in children. Patients should be advised to report visual disturbances immediately and to discontinue ethambutol pending visual evaluation. Ethambutol may precipitate attacks of gout. Although ethambutol crosses the placenta and teratogenicity has been observed in animals, problems in humans have not been documented.
Fixcom 4: Pyrazinamide: Liver function should be assessed before and regularly during treatment. It should be used with caution in patients with a history of gout. Caution should also be observed in patients with impaired renal function. Increased difficulty has been reported in controlling diabetes mellitus when diabetics are given by pyrazinamide.
Use in Pregnancy: Fixcom 2: A woman should be asked before starting TB treatment if she is pregnant. Most antituberculosis drugs are safe for use in pregnancy. A pregnant woman should be advised that successful treatment of TB with the recommended standardized regimen is important for successful outcome of pregnancy.
Fixcom 3: There are no adequate and well-controlled studies from the use of rifampicin, isoniazid and ethambutol on pregnancy and the fetus. Thus, these drugs should be used during pregnancy only if the benefit justifies the potential risk to the fetus.
Rifampicin: The International Union Against Tuberculosis and the WHO Expert Committee on Leprosy recommend treatment of pregnant patients with the same rifampicin-containing multidrug regimens as would be used in nonpregnant patients.
While administration of rifampicin to pregnant patients is generally considered to be safe, the drug does cross into the fetus and malformations and bleeding tendencies have been reported. It was considered that rifampicin did not increase the overall risk of congenital malformations.
Rifampicin treatment can increase the metabolism of vitamin K resulting in clotting disorders associated with vitamin K deficiency. Thus, it is recommended to have blood coagulation monitoring and prophylactic administration of vitamin K to mothers and neonates when the mother has received rifampicin during pregnancy.
Isoniazid: Isoniazid is recognized as being suitable for use in regimens for the treatment of tuberculosis in pregnant patients. Pyridoxine supplementation is recommended. Preventive therapy with isoniazid is generally delayed until after delivery unless other risk factors are present.
Ethambutol: Ethambutol crosses the placenta and is present in fetal tissue in amounts of at least 74.5% of the maternal serum concentration. Use of ethambutol during pregnancy has not been associated with fetal abnormalities. It is generally considered that the benefits of ethambutol in the treatment of tuberculosis outweigh any potential risks in pregnancy.
Use in Lactation: Fixcom 2: A breastfeeding woman who has TB should receive a full course of TB treatment. Timely and properly applied chemotherapy is the best way to prevent transmission of tubercle bacilli to her baby. All tuberculosis are compatible with breastfeeding; a woman taking them can safely continue to breastfeed. Mother and baby should stay together and the baby continue to be breastfed in the normal way, but be given prophylactic Isoniazid for at least 3 months beyond the time the mother is considered to be non-infectious. BCG vaccination of the newborn should be postponed until the end of isoniazid prophylaxis.
Fixcom 3: The use of these drugs during breastfeeding should be considered only if the expected benefit to the mother outweighs the potential risk to the infant.
Rifampicin is present in small amounts in breast milk. Mothers taking rifampicin may breastfeed.
Isoniazid is distributed into breast milk. Adverse effects on infants during breast feeding have not been reported, although such infants should be monitored for toxic reactions. Ethambutol diffuses into breast milk to produce concentrations similar to those in plasma.
Since isoniazid interacts with anticonvulsants used for epilepsy, it may be necessary to reduce the dosage of these drugs during treatment with isoniazid.
Rifampicin: Serious immunological reactions resulting in renal impairment, haemolysis or thrombocytopenia are on record in patients who resume taking rifampicin after a prolonged lapse of treatment. In this rare situation, it should be immediately and definitely withdrawn.
Careful monitoring of liver function is required in the elderly and in patients who are alcohol-dependent or have hepatic disease. Patients should be warned that treatment may produce reddish coloration of urine, tears, saliva and sputum and that contact lenses may be irreversibly stained.
Liver disorders: Isoniazid, rifampicin and pyrazinamide are all associated with hepatitis. Of the three drugs, rifampicin is least likely to cause hepatocellular damage, although it is associated
with cholestatic jaundice. Of the three agents, pyrazinamide is the most hepatotoxic.
Patients with the following conditions can receive the usual short-course chemotherapy regimens provided there is no clinical evidence of chronic liver disease: However, hepatotoxic reactions to antituberculosis drugs may be more common among these patients and should therefore be anticipated.
Established chronic liver disease: Patients with liver disease should not receive pyrazinamide. Isoniazid plus rifampicin plus one or two non-hepatotoxic drugs such as streptomycin and ethambutol can be used for a total treatment duration of 8 months. Alternative regimens are 9 Rifampicin/Ethambutol (RE) or Streptomycin/isoniazid Ethambutol (SHE) in the initial phase followed by Isoniazid/Ethambutol (HE) in the continuation phase. with a total treatment duration of 12 months. Recommended regimens are therefore 2SHRE/6HR. 9 RE or 2SHE/10HE.
Acute hepatitis (e.g. acute viral hepatitis): Uncommonly, a patient has TB and concurrently acute hepatitis unrelated to TB or TB treatment. Clinical judgement is necessary. In some cases, it is possible to defer TB treatment until the acute hepatitis has resolved. In other cases, when it is necessary to treat TB during acute hepatitis, the combination of Streptomycin/Ethambutol for 3 months is the safest option. If the hepatitis has resolved, the patient can then receive a continuation phase of 6 months isoniazid and rifampicin 6(HR). If the hepatitis has not resolved, Streptomycin/ethambutol should be continued for a total of 12 months.
Renal failure: Isoniazid, rifampicin and pyrazinamide are either eliminated almost entirely by biliary excretion or metabolized into non-toxic compounds. These drugs can therefore be given in normal dosage to patients with renal failure. Patients with severe renal failure should receive pyridoxine with isoniazid in order to prevent peripheral neuropathy.
Fixcom 3: Rifampicin: Liver functions should be checked before treatment with rifampicin and special care should be taken in alcoholic patients or those with preexisting liver disease who require regular monitoring during therapy. Rifampicin is contraindicated in patients with jaundice. A self-limiting hyperbilirubinemia may occur in the first 2 or 3 weeks of treatment. Alkaline phosphatase values may be raised moderately due to rifampicin's enzyme-inducing capacity. When other liver functions tests are within normal limits, hyperbilirubinemia in the 1st few weeks of moderately elevated alkaline phosphates are not indications to withdraw rifampicin. However, dose adjustment is necessary when there is other evidence of hepatic impairment and treatment should be suspended when there is evidence of more serious liver toxicity.
Blood counts should be monitored during prolonged treatment and in patients with hepatic disorders. Should thrombocytopenia or purpura occur then rifampicin should be withdrawn permanently. In patients who develop hemolytic anemia or renal failure, withdrawal of rifampicin is recommended.
Administration of rifampicin following interruption of treatment has been associated with increased risk of serious adverse effects.
Patients should be advised that rifampicin may color feces, saliva, sputum, sweat, tears, urine and other body fluids. Soft contact lenses worn by patients receiving rifampicin may become permanently stained.
Isoniazid: Isoniazid should be administered with caution to patients with convulsive disorders, a history of psychosis or hepatic or renal dysfunction. Patients who are at risk of neuropathy or pyridoxine deficiency, including those who are diabetic, alcoholic, malnourished, uremic, pregnant or HIV-infected, should receive pyridoxine usually in a dose of 10 mg daily, although some have suggested using up to 50 mg daily. If symptoms of hepatitis eg, malaise, fatigue, anorexia and nausea develop, isoniazid should be discontinued pending evaluation.
Liver function should be checked before treatment with isoniazid and special care should be taken in alcoholic patients or those with preexisting liver disease. Regular monitoring of liver function is recommended in patients with preexisting liver disease and isoniazid treatment should be suspended if serum aspartate aminotransferase concentrations are elevated to 3-5 times the normal upper limit or the bilirubin concentration rises. Periodic eye examination during isoniazid treatment have also been suggested.
Ethambutol: It should be used with great care in patients with visual defects, the elderly and in children whom evaluation changes in visual acuity may be difficult. Ocular examination is recommended before treatment with ethambutol and some consider regular examinations are necessary during treatment especially in children. Patients should be advised to report visual disturbances immediately and to discontinue ethambutol pending visual evaluation. Ethambutol may precipitate attacks of gout. Although ethambutol crosses the placenta and teratogenicity has been observed in animals, problems in humans have not been documented.
Fixcom 4: Pyrazinamide: Liver function should be assessed before and regularly during treatment. It should be used with caution in patients with a history of gout. Caution should also be observed in patients with impaired renal function. Increased difficulty has been reported in controlling diabetes mellitus when diabetics are given by pyrazinamide.
Use in Pregnancy: Fixcom 2: A woman should be asked before starting TB treatment if she is pregnant. Most antituberculosis drugs are safe for use in pregnancy. A pregnant woman should be advised that successful treatment of TB with the recommended standardized regimen is important for successful outcome of pregnancy.
Fixcom 3: There are no adequate and well-controlled studies from the use of rifampicin, isoniazid and ethambutol on pregnancy and the fetus. Thus, these drugs should be used during pregnancy only if the benefit justifies the potential risk to the fetus.
Rifampicin: The International Union Against Tuberculosis and the WHO Expert Committee on Leprosy recommend treatment of pregnant patients with the same rifampicin-containing multidrug regimens as would be used in nonpregnant patients.
While administration of rifampicin to pregnant patients is generally considered to be safe, the drug does cross into the fetus and malformations and bleeding tendencies have been reported. It was considered that rifampicin did not increase the overall risk of congenital malformations.
Rifampicin treatment can increase the metabolism of vitamin K resulting in clotting disorders associated with vitamin K deficiency. Thus, it is recommended to have blood coagulation monitoring and prophylactic administration of vitamin K to mothers and neonates when the mother has received rifampicin during pregnancy.
Isoniazid: Isoniazid is recognized as being suitable for use in regimens for the treatment of tuberculosis in pregnant patients. Pyridoxine supplementation is recommended. Preventive therapy with isoniazid is generally delayed until after delivery unless other risk factors are present.
Ethambutol: Ethambutol crosses the placenta and is present in fetal tissue in amounts of at least 74.5% of the maternal serum concentration. Use of ethambutol during pregnancy has not been associated with fetal abnormalities. It is generally considered that the benefits of ethambutol in the treatment of tuberculosis outweigh any potential risks in pregnancy.
Use in Lactation: Fixcom 2: A breastfeeding woman who has TB should receive a full course of TB treatment. Timely and properly applied chemotherapy is the best way to prevent transmission of tubercle bacilli to her baby. All tuberculosis are compatible with breastfeeding; a woman taking them can safely continue to breastfeed. Mother and baby should stay together and the baby continue to be breastfed in the normal way, but be given prophylactic Isoniazid for at least 3 months beyond the time the mother is considered to be non-infectious. BCG vaccination of the newborn should be postponed until the end of isoniazid prophylaxis.
Fixcom 3: The use of these drugs during breastfeeding should be considered only if the expected benefit to the mother outweighs the potential risk to the infant.
Rifampicin is present in small amounts in breast milk. Mothers taking rifampicin may breastfeed.
Isoniazid is distributed into breast milk. Adverse effects on infants during breast feeding have not been reported, although such infants should be monitored for toxic reactions. Ethambutol diffuses into breast milk to produce concentrations similar to those in plasma.
Use In Pregnancy & Lactation
Pregnancy: Fixcom 2: A woman should be asked before starting TB treatment if she is pregnant. Most antituberculosis drugs are safe for use in pregnancy. A pregnant woman should be advised that successful treatment of TB with the recommended standardized regimen is important for successful outcome of pregnancy.
Fixcom 3: There are no adequate and well-controlled studies from the use of rifampicin, isoniazid and ethambutol on pregnancy and the fetus. Thus, these drugs should be used during pregnancy only if the benefit justifies the potential risk to the fetus.
Rifampicin: The International Union Against Tuberculosis and the WHO Expert Committee on Leprosy recommend treatment of pregnant patients with the same rifampicin-containing multidrug regimens as would be used in nonpregnant patients.
While administration of rifampicin to pregnant patients is generally considered to be safe, the drug does cross into the fetus and malformations and bleeding tendencies have been reported. It was considered that rifampicin did not increase the overall risk of congenital malformations.
Rifampicin treatment can increase the metabolism of vitamin K resulting in clotting disorders associated with vitamin K deficiency. Thus, it is recommended to have blood coagulation monitoring and prophylactic administration of vitamin K to mothers and neonates when the mother has received rifampicin during pregnancy.
Isoniazid: Isoniazid is recognized as being suitable for use in regimens for the treatment of tuberculosis in pregnant patients. Pyridoxine supplementation is recommended. Preventive therapy with isoniazid is generally delayed until after delivery unless other risk factors are present.
Ethambutol: Ethambutol crosses the placenta and is present in fetal tissue in amounts of at least 74.5% of the maternal serum concentration. Use of ethambutol during pregnancy has not been associated with fetal abnormalities. It is generally considered that the benefits of ethambutol in the treatment of tuberculosis outweigh any potential risks in pregnancy.
Breastfeeding: Fixcom 2: A breastfeeding woman who has TB should receive a full course of TB treatment. Timely and properly applied chemotherapy is the best way to prevent transmission of tubercle bacilli to her baby. All tuberculosis are compatible with breastfeeding; a woman taking them can safely continue to breastfeed. Mother and baby should stay together and the baby continue to be breastfed in the normal way, but be given prophylactic Isoniazid for at least 3 months beyond the time the mother is considered to be non-infectious. BCG vaccination of the newborn should be postponed until the end of isoniazid prophylaxis.
Fixcom 3: The use of these drugs during breastfeeding should be considered only if the expected benefit to the mother outweighs the potential risk to the infant.
Rifampicin is present in small amounts in breast milk. Mothers taking rifampicin may breastfeed.
Isoniazid is distributed into breast milk. Adverse effects on infants during breast feeding have not been reported, although such infants should be monitored for toxic reactions. Ethambutol diffuses into breast milk to produce concentrations similar to those in plasma.
Oral Contraception: Rifampicin interacts with oral contraceptive medications with a risk of deceased protective efficacy against pregnancy. A woman receiving oral contraception may choose between two options while receiving treatment with rifampicin: following consultation with a clinician, an oral contraceptive pill containing a higher dose of estrogen (5Oug) may be taken. or another form of contraception used.
Fixcom 3: There are no adequate and well-controlled studies from the use of rifampicin, isoniazid and ethambutol on pregnancy and the fetus. Thus, these drugs should be used during pregnancy only if the benefit justifies the potential risk to the fetus.
Rifampicin: The International Union Against Tuberculosis and the WHO Expert Committee on Leprosy recommend treatment of pregnant patients with the same rifampicin-containing multidrug regimens as would be used in nonpregnant patients.
While administration of rifampicin to pregnant patients is generally considered to be safe, the drug does cross into the fetus and malformations and bleeding tendencies have been reported. It was considered that rifampicin did not increase the overall risk of congenital malformations.
Rifampicin treatment can increase the metabolism of vitamin K resulting in clotting disorders associated with vitamin K deficiency. Thus, it is recommended to have blood coagulation monitoring and prophylactic administration of vitamin K to mothers and neonates when the mother has received rifampicin during pregnancy.
Isoniazid: Isoniazid is recognized as being suitable for use in regimens for the treatment of tuberculosis in pregnant patients. Pyridoxine supplementation is recommended. Preventive therapy with isoniazid is generally delayed until after delivery unless other risk factors are present.
Ethambutol: Ethambutol crosses the placenta and is present in fetal tissue in amounts of at least 74.5% of the maternal serum concentration. Use of ethambutol during pregnancy has not been associated with fetal abnormalities. It is generally considered that the benefits of ethambutol in the treatment of tuberculosis outweigh any potential risks in pregnancy.
Breastfeeding: Fixcom 2: A breastfeeding woman who has TB should receive a full course of TB treatment. Timely and properly applied chemotherapy is the best way to prevent transmission of tubercle bacilli to her baby. All tuberculosis are compatible with breastfeeding; a woman taking them can safely continue to breastfeed. Mother and baby should stay together and the baby continue to be breastfed in the normal way, but be given prophylactic Isoniazid for at least 3 months beyond the time the mother is considered to be non-infectious. BCG vaccination of the newborn should be postponed until the end of isoniazid prophylaxis.
Fixcom 3: The use of these drugs during breastfeeding should be considered only if the expected benefit to the mother outweighs the potential risk to the infant.
Rifampicin is present in small amounts in breast milk. Mothers taking rifampicin may breastfeed.
Isoniazid is distributed into breast milk. Adverse effects on infants during breast feeding have not been reported, although such infants should be monitored for toxic reactions. Ethambutol diffuses into breast milk to produce concentrations similar to those in plasma.
Oral Contraception: Rifampicin interacts with oral contraceptive medications with a risk of deceased protective efficacy against pregnancy. A woman receiving oral contraception may choose between two options while receiving treatment with rifampicin: following consultation with a clinician, an oral contraceptive pill containing a higher dose of estrogen (5Oug) may be taken. or another form of contraception used.
Adverse Reactions
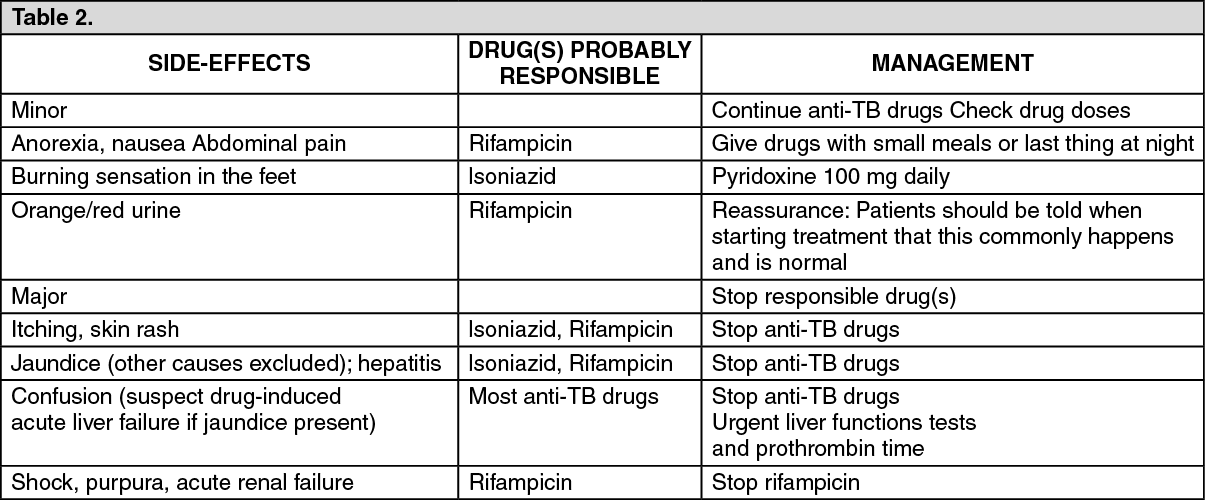
Fixcom 2: Most TB patients complete their treatment without any significant adverse effects of drugs. However, a few patients do experience adverse effects. It is therefore important that patients be clinically monitored during treatment so that adverse effects can be detected promptly and managed properly. Routine laboratory monitoring is not necessary.
Health personnel can monitor adverse effects of drugs by teaching patients how to recognize symptoms of common adverse effects and to report if they develop such symptoms, and by asking about symptoms when patients report to collect drugs.
In general, a patient who develops minor adverse effects should continue the TB treatment, sometimes at a reduced dose. The patient also receives symptomatic treatment. If a patient develops a major side effect, the treatment or the offending drug is stopped. Further management depends on the nature of the adverse reaction.
Patients with major adverse reactions should be managed in a hospital. (See Table 2).
Health personnel can monitor adverse effects of drugs by teaching patients how to recognize symptoms of common adverse effects and to report if they develop such symptoms, and by asking about symptoms when patients report to collect drugs.
In general, a patient who develops minor adverse effects should continue the TB treatment, sometimes at a reduced dose. The patient also receives symptomatic treatment. If a patient develops a major side effect, the treatment or the offending drug is stopped. Further management depends on the nature of the adverse reaction.
Patients with major adverse reactions should be managed in a hospital. (See Table 2).
Fixcom 3: Rifampicin: Rifampicin is usually well-tolerated. Adverse effects are more common during intermittent therapy or after restarting interrupted treatment.
Some patients may experience a cutaneous syndrome which presents 2-3 hrs after a daily or intermittent dose eg, facial flushing, itching, rash or rarely, eye irritation. A 12-hr "flu" syndrome of fever, chills, bone pains, shortness of breath and malaise has been associated with intermittent administration. It usually occurs after 3-6 months of intermittent administration and has a higher incidence with doses of ≥20 mg/kg body weight given once weekly than with currently recommended regimens. Anaphylaxis or shock has occurred rarely.
GI adverse effects include nausea, vomiting, anorexia, diarrhea and epigastric distress. GI bleeding and erosive gastritis, ulcerative and eosinophilic colitis have been reported. Administration on an empty stomach is recommended for maximal absorption, but this has to be balanced against administration after a meal to minimize GI intolerance. Pseudomembranous colitis has been reported. Rifampicin produces transient abnormalities in liver function. Hepatitis occurs rarely. Fatalities due to hepatotoxicity have been reported occasionally. Rifampicin can cause thrombocytopenia and purpura, usually when administered as an intermittent regiment and if this occurs, further administration of rifampicin is contraindicated. Other hematological adverse effects include eosinophilia, leucopenia and hemolytic anemia.
Alterations in kidney function and renal failure have occurred, particularly during intermittent therapy. Menstrual disturbances have been reported.
Nervous system adverse effects include headache, drowsiness, ataxia, dizziness and numbness.
Edema, myopathy and muscular weakness have been reported.
Rifampicin causes a harmless orange-red discoloration of the urine and other body fluids.
Isoniazid: Isoniazid is generally well-tolerated at currently recommended doses. However, patients who are slow acetylators of isoniazid appear to have a higher incidence of some adverse effects. Also, patients whose nutrition is poor are at risk of peripheral neuritis which is 1 of the commonest adverse effects of isoniazid. Other neurological adverse effects include psychotic reactions and convulsions. Pyridoxine may be given to prevent or treat these adverse effects. Transient increase in liver enzymes occur in 10-20% of patients during the 1st few months and usually return to normal despite continued treatment. Elevated liver enzymes associated with clinical signs of hepatitis eg, nausea and vomiting or fatigue may indicate hepatic damage: In these circumstances, isoniazid should be stopped pending evaluation and should only be reintroduced cautiously once hepatic functions has recovered. The incidence of liver damage is highest in patients >35 years. The influence of acetylator status is uncertain. Fatalities have occurred following liver necrosis. Hematological effects reported following use of isoniazid include various anemias, agranulocytosis, thrombocytopenia and eosinophilia.
Hypersensitivity reactions occur infrequently and include skin eruptions (including erythema multiforme), fever and vasculitis.
Other adverse effects include nausea, vomiting, pellagra, purpura, hyperglycemia, lupus-like syndrome, urinary retention and gynecomastia.
Ethambutol: The most important adverse effect of ethambutol is retrobulbar neuritis with a reduction in visual acuity, constriction of visual field, central or peripheral scotoma and green-red color blindness. One or both eyes may be affected. The degree of visual color blindness. One or both eyes may be affected. The degree of visual impairment appears to depend on the dose and duration of therapy; toxicity is observed most frequently at daily doses of 25 mg/kg body weight and after 2 months of therapy. Recovery of vision usually takes place over a period of a few weeks or months, but in rare cases, it may take up to ≥1 year or the effect may be permanent. Retinal hemorrhage has occurred rarely.
Renal clearance of urate may be reduced and acute gout has been precipitated rarely.
Hypersensitivity reactions including skin rashes, pruritus, leucopenia, fever and joint pains have occurred but appear to be rare with ethambutol. Other adverse effects which have been reported include confusion, disorientation, hallucinations, headache, dizziness, malaise, jaundice or transient liver dysfunction, peripheral neuritis, thrombocytopenia, pulmonary infiltrates, eosinophilia and GI disturbances eg, nausea, vomiting, anorexia and abdominal pain.
Fixcom 4: Pyrazinamide: Hepatotoxicity is the most serious side effect of pyrazinamide therapy and its frequency appears to be dose-related. However, in currently recommended dose, when given with isoniazid and rifampicin, the incidence of hepatitis has been reported to be <3%. Patients may experience transient increase in liver enzyme values, more seriously hepatomegaly, splenomegaly and jaundice may develop and on rare occasions, death has occurred. Hyperuricemia commonly occurs and may lead to attacks of gout. Other side effects are anorexia, nausea, vomiting, arthralgia, malaise, fever, sideroblastic anemia and dysuria. Photosensitivity and skin rashes have been reported on rare occasions.
Some patients may experience a cutaneous syndrome which presents 2-3 hrs after a daily or intermittent dose eg, facial flushing, itching, rash or rarely, eye irritation. A 12-hr "flu" syndrome of fever, chills, bone pains, shortness of breath and malaise has been associated with intermittent administration. It usually occurs after 3-6 months of intermittent administration and has a higher incidence with doses of ≥20 mg/kg body weight given once weekly than with currently recommended regimens. Anaphylaxis or shock has occurred rarely.
GI adverse effects include nausea, vomiting, anorexia, diarrhea and epigastric distress. GI bleeding and erosive gastritis, ulcerative and eosinophilic colitis have been reported. Administration on an empty stomach is recommended for maximal absorption, but this has to be balanced against administration after a meal to minimize GI intolerance. Pseudomembranous colitis has been reported. Rifampicin produces transient abnormalities in liver function. Hepatitis occurs rarely. Fatalities due to hepatotoxicity have been reported occasionally. Rifampicin can cause thrombocytopenia and purpura, usually when administered as an intermittent regiment and if this occurs, further administration of rifampicin is contraindicated. Other hematological adverse effects include eosinophilia, leucopenia and hemolytic anemia.
Alterations in kidney function and renal failure have occurred, particularly during intermittent therapy. Menstrual disturbances have been reported.
Nervous system adverse effects include headache, drowsiness, ataxia, dizziness and numbness.
Edema, myopathy and muscular weakness have been reported.
Rifampicin causes a harmless orange-red discoloration of the urine and other body fluids.
Isoniazid: Isoniazid is generally well-tolerated at currently recommended doses. However, patients who are slow acetylators of isoniazid appear to have a higher incidence of some adverse effects. Also, patients whose nutrition is poor are at risk of peripheral neuritis which is 1 of the commonest adverse effects of isoniazid. Other neurological adverse effects include psychotic reactions and convulsions. Pyridoxine may be given to prevent or treat these adverse effects. Transient increase in liver enzymes occur in 10-20% of patients during the 1st few months and usually return to normal despite continued treatment. Elevated liver enzymes associated with clinical signs of hepatitis eg, nausea and vomiting or fatigue may indicate hepatic damage: In these circumstances, isoniazid should be stopped pending evaluation and should only be reintroduced cautiously once hepatic functions has recovered. The incidence of liver damage is highest in patients >35 years. The influence of acetylator status is uncertain. Fatalities have occurred following liver necrosis. Hematological effects reported following use of isoniazid include various anemias, agranulocytosis, thrombocytopenia and eosinophilia.
Hypersensitivity reactions occur infrequently and include skin eruptions (including erythema multiforme), fever and vasculitis.
Other adverse effects include nausea, vomiting, pellagra, purpura, hyperglycemia, lupus-like syndrome, urinary retention and gynecomastia.
Ethambutol: The most important adverse effect of ethambutol is retrobulbar neuritis with a reduction in visual acuity, constriction of visual field, central or peripheral scotoma and green-red color blindness. One or both eyes may be affected. The degree of visual color blindness. One or both eyes may be affected. The degree of visual impairment appears to depend on the dose and duration of therapy; toxicity is observed most frequently at daily doses of 25 mg/kg body weight and after 2 months of therapy. Recovery of vision usually takes place over a period of a few weeks or months, but in rare cases, it may take up to ≥1 year or the effect may be permanent. Retinal hemorrhage has occurred rarely.
Renal clearance of urate may be reduced and acute gout has been precipitated rarely.
Hypersensitivity reactions including skin rashes, pruritus, leucopenia, fever and joint pains have occurred but appear to be rare with ethambutol. Other adverse effects which have been reported include confusion, disorientation, hallucinations, headache, dizziness, malaise, jaundice or transient liver dysfunction, peripheral neuritis, thrombocytopenia, pulmonary infiltrates, eosinophilia and GI disturbances eg, nausea, vomiting, anorexia and abdominal pain.
Fixcom 4: Pyrazinamide: Hepatotoxicity is the most serious side effect of pyrazinamide therapy and its frequency appears to be dose-related. However, in currently recommended dose, when given with isoniazid and rifampicin, the incidence of hepatitis has been reported to be <3%. Patients may experience transient increase in liver enzyme values, more seriously hepatomegaly, splenomegaly and jaundice may develop and on rare occasions, death has occurred. Hyperuricemia commonly occurs and may lead to attacks of gout. Other side effects are anorexia, nausea, vomiting, arthralgia, malaise, fever, sideroblastic anemia and dysuria. Photosensitivity and skin rashes have been reported on rare occasions.
Drug Interactions
Fixcom 2: Isoniazid tends raise plasma concentrations of phenytoin and carbamazepine by inhibiting their metabolism in the liver. The absorption of isoniazid is impaired by aluminum hydroxide.
Rifampicin induces hepatic enzymes, and may increase the dosage requirements of drugs metabolized in the liver. These include corticosteroids, steroid contraceptives, oral hypoglycaemic agents, oral anticoagulants, phenytoin, cimetidine, cyclosporine and digitalisglycosides. Since rifampicin reduce the effectiveness of oral contraceptives, women should be advised to choose between one of the following options for contraception. Following consultation with a clinician, the patient may use an oral contraceptive pill containing a higher dose of estrogen (50 µg). Alternatively, a nonhormonal method of contraception may be used throughout rifampicin treatment and for at least one month subsequently.
Current antiretroviral drugs interact with rifampicin. This may result ineffectiveness of antiretroviral drugs, ineffective treatment of TB or an increased risk of drug toxicity. Biliary excretion of radiocontrast media and sulfobromopthalein sodium may be reduced and microbiological assays for folic acid and vitamin B12 disturbed.
Fixcom 3: Rifampicin: Rifampicin accelerates the metabolism of some drugs by inducing the microsomal liver enzymes and possibly interfering with hepatic uptake. Although most drugs involved may require an increase in dosage to maintain effectiveness, women taking oral contraceptives should change to another form of contraception.
The absorption of rifampicin may be reduced by administration with antacids, drugs that reduce gastric motility (anticholinergics and opioids), ketoconazole or preparations containing bentonite. However, such reactions can be overcome by giving rifampicin in a few hrs before any of these drugs.
Isoniazid: The risk of hepatotoxicity may be increased in patients receiving isoniazid in combination with rifampicin or other potentially hepatotoxic drugs.
Isoniazid can inhibit the hepatic metabolism of a number of drugs, in some cases leading to increased toxicity. These include the antiepileptics carbamazepine, ethosuximide and phenytoin, the benzodiazepines diazepam, triazolam, chlorzoxazone and theophylline. The metabolism of enflurane may be increased in patients receiving isoniazid resulting in potentially nephrotoxic levels of fluoride. Isoniazid has been associated with increased concentrations or toxicity of clofazimine, cycloserine and warfarins.
The metabolism of isoniazid may be increased in chronic alcoholics; this may lead to reduced isoniazid effectiveness. These patients may also be at increased risk of developing isoniazid-induced peripheral neuropathies and hepatic damage.
Oral absorption of isoniazid is reduced by aluminum-containing antacids; isoniazid should be given 1 hr before the antacid.
Fixcom 4: Pyrazinamide: Probenecid is known to block the excretion of pyrazinamide.
Rifampicin induces hepatic enzymes, and may increase the dosage requirements of drugs metabolized in the liver. These include corticosteroids, steroid contraceptives, oral hypoglycaemic agents, oral anticoagulants, phenytoin, cimetidine, cyclosporine and digitalisglycosides. Since rifampicin reduce the effectiveness of oral contraceptives, women should be advised to choose between one of the following options for contraception. Following consultation with a clinician, the patient may use an oral contraceptive pill containing a higher dose of estrogen (50 µg). Alternatively, a nonhormonal method of contraception may be used throughout rifampicin treatment and for at least one month subsequently.
Current antiretroviral drugs interact with rifampicin. This may result ineffectiveness of antiretroviral drugs, ineffective treatment of TB or an increased risk of drug toxicity. Biliary excretion of radiocontrast media and sulfobromopthalein sodium may be reduced and microbiological assays for folic acid and vitamin B12 disturbed.
Fixcom 3: Rifampicin: Rifampicin accelerates the metabolism of some drugs by inducing the microsomal liver enzymes and possibly interfering with hepatic uptake. Although most drugs involved may require an increase in dosage to maintain effectiveness, women taking oral contraceptives should change to another form of contraception.
The absorption of rifampicin may be reduced by administration with antacids, drugs that reduce gastric motility (anticholinergics and opioids), ketoconazole or preparations containing bentonite. However, such reactions can be overcome by giving rifampicin in a few hrs before any of these drugs.
Isoniazid: The risk of hepatotoxicity may be increased in patients receiving isoniazid in combination with rifampicin or other potentially hepatotoxic drugs.
Isoniazid can inhibit the hepatic metabolism of a number of drugs, in some cases leading to increased toxicity. These include the antiepileptics carbamazepine, ethosuximide and phenytoin, the benzodiazepines diazepam, triazolam, chlorzoxazone and theophylline. The metabolism of enflurane may be increased in patients receiving isoniazid resulting in potentially nephrotoxic levels of fluoride. Isoniazid has been associated with increased concentrations or toxicity of clofazimine, cycloserine and warfarins.
The metabolism of isoniazid may be increased in chronic alcoholics; this may lead to reduced isoniazid effectiveness. These patients may also be at increased risk of developing isoniazid-induced peripheral neuropathies and hepatic damage.
Oral absorption of isoniazid is reduced by aluminum-containing antacids; isoniazid should be given 1 hr before the antacid.
Fixcom 4: Pyrazinamide: Probenecid is known to block the excretion of pyrazinamide.
Storage
Store at room temperatures not exceeding 30°C.
Action
Pharmacology: Pharmacodynamics: There are three main properties of antituberculosis drugs: bactericidal activity; sterilizing activity and the ability to prevent resistance. The essential antituberculosis drugs possess these properties to different extents. Isoniazid and rifampicin are the most powerful bactericidal drugs, active against all populations to TB bacilli. Rifampicin is the most potent sterilizing drug available.
Pharmacokinetics: Rifampicin: Rifampicin is readily absorbed from the GIT and peak plasma concentrations of about 7-10 mcg/mL have been reported 2-4 hrs after a dose of 600 mg, although there may be considerable interindividual variation. Food may reduce and delay absorption. Rifampicin is approximately 80% bound to plasma proteins. It is widely distributed in body tissues and fluids and diffusion into the CSF is increased when the meninges are inflamed. Rifampicin crosses the placenta and is distributed into breast milk. Half-lives for rifampicin have been reported to range initially from 2-5 hrs, the longest elimination times occurring after the largest doses. However, as rifampicin induces its own metabolism, elimination time may decrease by up to 40% during the first 2 weeks, resulting in t½ of about 1-3 hrs. The t½ is prolonged in patients with liver disease.
Rifampicin is rapidly metabolized in the liver mainly to active 25-O-deacetyrifampicin; rifampicin and deacetylrifampicin are excreted in the bile. Deacetylation diminishes intestinal reabsorption and increases fecal excretion, although significant enterohepatic circulation still takes place. About 60% of a dose eventually appears in the feces. The amount excreted in the urine increases with increasing doses and up to 30% of a dose of 900 mg may be excreted in the urine, about half of it within 24 hrs. The metabolite formylrifampicin is also excreted in the urine. In patients with impaired renal function, the t½ of rifampicin is not prolonged at doses of ≤600 mg.
Isoniazid: Isoniazid is readily absorbed from the GIT. Peak concentrations of about 3-8 mcg/mL appear in blood 1-2 hrs after a fasting dose of 300 mg orally. The rate and extent of absorption of isoniazid is reduced by food. Isoniazid is not considered to be bound appreciably to plasma proteins and diffuses into all body tissues and fluids, including the CSF. The plasma t½ for isoniazid ranges from about 1-6 hrs, those who are fast acetylators having shorter t½. The primary metabolic route is the acetylation of isoniazid to acetylisoniazid by N-acetyltransferase found in the liver and small intestine.
In patients with normal renal function, over 75% of a dose appears in the urine in 24 hrs, mainly as metabolites. Small amounts of drug are also excreted in the feces. Isoniazid is removed by dialysis.
Ethambutol: About 80% of an oral dose is absorbed from the GIT and the remainder appears in the feces unchanged. Absorption is not significantly impaired by food. After a single dose of 25 mg/kg body weight, peak plasma concentrations of up to 5 mcg/mL appear within 4 hrs and are <1 mcg/mL by 24 hrs.
Ethambutol is distributed to most tissues including the lungs, kidneys and erythrocytes. It diffuses into the CSF when the meninges are inflamed. It has been reported to cross the placenta and is distributed into breast milk. The elimination t½ following oral administration is about 3-4 hrs.
Ethambutol is partially metabolized in the liver to the aldehyde and dicarboxylic acid derivatives which are inactive and then excreted in the urine. Most of a dose appears in the urine within 24 hrs as unchanged drug and 8-15% as the inactive metabolites. About 20% of the dose is excreted unchanged in the feces.
Although the absorption of ethambutol is not generally regarded as being impaired by food, a study in 14 healthy subjects suggested that administration with a high fat meal or an antacid could delay absorption and reduce the maximum plasma concentration.
Fixcom 4: Pyrazinamide: Pyrazinamide is readily absorbed from the GIT. Peak serum concentrations occur about 2 hrs after a dose orally and have been reported to be about 35 mcg/mL after 1.5 g and 66 mcg/mL after 3 g. Pyrazinamide is widely distributed in the body fluids and tissues and diffuses into the CSF. The t½ has been reported to be about 9-10 hrs. It is metabolized primarily in the liver by hydrolysis to the major active metabolite pyrazinoic acid which is subsequently hydroxylated to the major excretory product 5-hydroxypyrazinoic acid. It is excreted through the kidney mainly by glomerular filtration. About 70% of the dose appears in the urine within 24 hrs mainly as metabolites and 4-14% as unchanged drug. Pyrazinamide is removed by dialysis.
Microbiology: Antimicrobial Actions: Rifampicin: Rifampicin is bactericidal against a wide range of microorganisms and interferes with their synthesis of nucleic acids by inhibiting DNA-dependent RNA polymerase. It has the ability to kill intracellular organisms. It is active against mycobacteria, including Mycobacterium tuberculosis and M. leprae and having high sterilizing activity against these organisms, it possesses the ability to eliminate semi-dormant or persisting organisms. Rifampicin is active against gram-positive bacteria, especially staphylococci, but less active against gram-negative organisms. The most sensitive gram-negative bacteria include Neisseria meningitides, N. gonorrhoeae, Haemophilus influenzae and Legionella spp. Rifampicin also has activity against Chlamydia trachomatis and some anaerobic bacteria. At high concentrations, it is active against some viruses. Rifampicin has no effect on fungi but has been reported to enhance the antifungal activity of amphotericin B. Minimum inhibitory concentrations (MICs) tend to vary with the medium used; MICs for the most sensitive organisms (Chlamydia, staphylococci) tend to range from about 0.01-0.02 mcg/mL, while the MIC for most susceptible mycobacteria ranges from 0.1-0.2 mcg/mL. The concomitant use of other antimicrobials may enhance or antagonize the bactericidal activity of rifampicin.
Strains of Mycobacterium tuberculosis, M. leprae and other usually susceptible bacteria gave demonstrated resistance, both initially and during treatment. Thus in tuberculosis and leprosy regiments, rifampicin is used in combination with other drugs to delay or prevent the development of rifampicin resistance.
Isoniazid: Isoniazid is highly active against Mycobacterium tuberculosis which it inhibits in vitro at concentrations of 0.02-0.2 mcg/mL. Isoniazid may have activity against some strains of other mycobacteria including M. kansasii.
Although it is rapidly bactericidal against actively dividing M. tuberculosis, it is considered to be only bacteriostatic against semi-dormant organisms and has less sterilizing activity than rifampicin or pyrazinamide.
Resistance to isoniazid develops rapidly if it is used alone in the treatment of clinical infection and may be due in some strains to loss of the gene for catalase production. Resistance is delayed or prevented by combination with other antimycobacterials and it appears to be highly effective in preventing emergence of resistance to other antituberculous drugs. Resistance does not appear to be a problem when isoniazid is used alone in prophylaxis, probably because the bacillary load is low.
Ethambutol: Ethambutol is bacteriostatic against Mycobacterium tuberculosis with an MIC of 0.5-0.8 mcg/mL; it is bactericidal at higher concentrations. It possesses little sterilizing activity. Resistant strains of M. tuberculosis are readily produced if ethambutol is used alone.
Fixcom 4: Pyrazinamide: Pyrazinamide has a bactericidal effect on Mycobacterium tuberculosis but appears to have no activity against other mycobacteria or microorganisms in vitro. The MIC for M. tuberculosis is <20 mcg/mL at pH 5.6; it is almost completely inactive at neutral pH. Pyrazinamide is effective against persisting tubercle bacilli within the acidic intracellular environment of the macrophages. The initial inflammatory response to chemotherapy increases the number of organisms in the acidic environment. As inflammation subsides and pH increase, the sterilizing activity of pyrazinamide decreases. This pH-dependent activity explains the clinical effectiveness of pyrazinamide as part of the initial 8-week phase in short-course treatment regimens.
Pharmacokinetics: Rifampicin: Rifampicin is readily absorbed from the GIT and peak plasma concentrations of about 7-10 mcg/mL have been reported 2-4 hrs after a dose of 600 mg, although there may be considerable interindividual variation. Food may reduce and delay absorption. Rifampicin is approximately 80% bound to plasma proteins. It is widely distributed in body tissues and fluids and diffusion into the CSF is increased when the meninges are inflamed. Rifampicin crosses the placenta and is distributed into breast milk. Half-lives for rifampicin have been reported to range initially from 2-5 hrs, the longest elimination times occurring after the largest doses. However, as rifampicin induces its own metabolism, elimination time may decrease by up to 40% during the first 2 weeks, resulting in t½ of about 1-3 hrs. The t½ is prolonged in patients with liver disease.
Rifampicin is rapidly metabolized in the liver mainly to active 25-O-deacetyrifampicin; rifampicin and deacetylrifampicin are excreted in the bile. Deacetylation diminishes intestinal reabsorption and increases fecal excretion, although significant enterohepatic circulation still takes place. About 60% of a dose eventually appears in the feces. The amount excreted in the urine increases with increasing doses and up to 30% of a dose of 900 mg may be excreted in the urine, about half of it within 24 hrs. The metabolite formylrifampicin is also excreted in the urine. In patients with impaired renal function, the t½ of rifampicin is not prolonged at doses of ≤600 mg.
Isoniazid: Isoniazid is readily absorbed from the GIT. Peak concentrations of about 3-8 mcg/mL appear in blood 1-2 hrs after a fasting dose of 300 mg orally. The rate and extent of absorption of isoniazid is reduced by food. Isoniazid is not considered to be bound appreciably to plasma proteins and diffuses into all body tissues and fluids, including the CSF. The plasma t½ for isoniazid ranges from about 1-6 hrs, those who are fast acetylators having shorter t½. The primary metabolic route is the acetylation of isoniazid to acetylisoniazid by N-acetyltransferase found in the liver and small intestine.
In patients with normal renal function, over 75% of a dose appears in the urine in 24 hrs, mainly as metabolites. Small amounts of drug are also excreted in the feces. Isoniazid is removed by dialysis.
Ethambutol: About 80% of an oral dose is absorbed from the GIT and the remainder appears in the feces unchanged. Absorption is not significantly impaired by food. After a single dose of 25 mg/kg body weight, peak plasma concentrations of up to 5 mcg/mL appear within 4 hrs and are <1 mcg/mL by 24 hrs.
Ethambutol is distributed to most tissues including the lungs, kidneys and erythrocytes. It diffuses into the CSF when the meninges are inflamed. It has been reported to cross the placenta and is distributed into breast milk. The elimination t½ following oral administration is about 3-4 hrs.
Ethambutol is partially metabolized in the liver to the aldehyde and dicarboxylic acid derivatives which are inactive and then excreted in the urine. Most of a dose appears in the urine within 24 hrs as unchanged drug and 8-15% as the inactive metabolites. About 20% of the dose is excreted unchanged in the feces.
Although the absorption of ethambutol is not generally regarded as being impaired by food, a study in 14 healthy subjects suggested that administration with a high fat meal or an antacid could delay absorption and reduce the maximum plasma concentration.
Fixcom 4: Pyrazinamide: Pyrazinamide is readily absorbed from the GIT. Peak serum concentrations occur about 2 hrs after a dose orally and have been reported to be about 35 mcg/mL after 1.5 g and 66 mcg/mL after 3 g. Pyrazinamide is widely distributed in the body fluids and tissues and diffuses into the CSF. The t½ has been reported to be about 9-10 hrs. It is metabolized primarily in the liver by hydrolysis to the major active metabolite pyrazinoic acid which is subsequently hydroxylated to the major excretory product 5-hydroxypyrazinoic acid. It is excreted through the kidney mainly by glomerular filtration. About 70% of the dose appears in the urine within 24 hrs mainly as metabolites and 4-14% as unchanged drug. Pyrazinamide is removed by dialysis.
Microbiology: Antimicrobial Actions: Rifampicin: Rifampicin is bactericidal against a wide range of microorganisms and interferes with their synthesis of nucleic acids by inhibiting DNA-dependent RNA polymerase. It has the ability to kill intracellular organisms. It is active against mycobacteria, including Mycobacterium tuberculosis and M. leprae and having high sterilizing activity against these organisms, it possesses the ability to eliminate semi-dormant or persisting organisms. Rifampicin is active against gram-positive bacteria, especially staphylococci, but less active against gram-negative organisms. The most sensitive gram-negative bacteria include Neisseria meningitides, N. gonorrhoeae, Haemophilus influenzae and Legionella spp. Rifampicin also has activity against Chlamydia trachomatis and some anaerobic bacteria. At high concentrations, it is active against some viruses. Rifampicin has no effect on fungi but has been reported to enhance the antifungal activity of amphotericin B. Minimum inhibitory concentrations (MICs) tend to vary with the medium used; MICs for the most sensitive organisms (Chlamydia, staphylococci) tend to range from about 0.01-0.02 mcg/mL, while the MIC for most susceptible mycobacteria ranges from 0.1-0.2 mcg/mL. The concomitant use of other antimicrobials may enhance or antagonize the bactericidal activity of rifampicin.
Strains of Mycobacterium tuberculosis, M. leprae and other usually susceptible bacteria gave demonstrated resistance, both initially and during treatment. Thus in tuberculosis and leprosy regiments, rifampicin is used in combination with other drugs to delay or prevent the development of rifampicin resistance.
Isoniazid: Isoniazid is highly active against Mycobacterium tuberculosis which it inhibits in vitro at concentrations of 0.02-0.2 mcg/mL. Isoniazid may have activity against some strains of other mycobacteria including M. kansasii.
Although it is rapidly bactericidal against actively dividing M. tuberculosis, it is considered to be only bacteriostatic against semi-dormant organisms and has less sterilizing activity than rifampicin or pyrazinamide.
Resistance to isoniazid develops rapidly if it is used alone in the treatment of clinical infection and may be due in some strains to loss of the gene for catalase production. Resistance is delayed or prevented by combination with other antimycobacterials and it appears to be highly effective in preventing emergence of resistance to other antituberculous drugs. Resistance does not appear to be a problem when isoniazid is used alone in prophylaxis, probably because the bacillary load is low.
Ethambutol: Ethambutol is bacteriostatic against Mycobacterium tuberculosis with an MIC of 0.5-0.8 mcg/mL; it is bactericidal at higher concentrations. It possesses little sterilizing activity. Resistant strains of M. tuberculosis are readily produced if ethambutol is used alone.
Fixcom 4: Pyrazinamide: Pyrazinamide has a bactericidal effect on Mycobacterium tuberculosis but appears to have no activity against other mycobacteria or microorganisms in vitro. The MIC for M. tuberculosis is <20 mcg/mL at pH 5.6; it is almost completely inactive at neutral pH. Pyrazinamide is effective against persisting tubercle bacilli within the acidic intracellular environment of the macrophages. The initial inflammatory response to chemotherapy increases the number of organisms in the acidic environment. As inflammation subsides and pH increase, the sterilizing activity of pyrazinamide decreases. This pH-dependent activity explains the clinical effectiveness of pyrazinamide as part of the initial 8-week phase in short-course treatment regimens.
MedsGo Class
Anti-TB Agents
Features
Dosage
150mg / 275mg / 75mg
Ingredients
- Ethambutol
- Isoniazid
- Rifampicin
Packaging
Film-Coated Tablet 1's
Generic Name
Ethambutol / Isoniazid / Rifampicin
Registration Number
DRP-1432
Classification
Prescription Drug (RX)
Reviews
No reviews found
Product Questions
Questions








