Indications/Uses
For the prevention and treatment of allergic rhinitis.
For the prevention of recurrence of nasal polyps after surgical removal.
For the prevention of recurrence of nasal polyps after surgical removal.
Dosage/Direction for Use
See table.

Overdosage
Chronic overdosage may lead to adrenocortical suppression. There was no evidence of toxicity observed in healthy adults given intranasal fluticasone propionate 2 mg twice daily for 7 days (10 times the recommended dosage).
Contraindications
Hypersensitivity to any ingredient in the product.
Special Precautions
Intranasal corticosteroids may cause reduction in growth velocity when administered to children.
Avoid higher than recommended doses of fluticasone propionate nasal spray since hypercorticism and suppression of the hypothalamic-pituitary-adrenal (HPA) axis function may occur.
Patients who have received systemic corticosteroids for prolonged periods and transferred to topical corticosteroids should be monitored carefully since corticosteroid withdrawal symptoms (e.g., joint pain, muscular pain, lassitude, depression), acute adrenal insufficiency, or severe symptomatic exacerbation of asthma or other clinical conditions may occur.
Concomitant use of intranasal corticosteroids with other inhaled steroids may increase the risk of manifestations of hypercorticism and/or suppression of HPA axis function.
Although there have been no reports of manifestations of Cushing's syndrome (e.g., hypertension, glucose intolerance, cushingoid features) associated with intranasal fluticasone propionate therapy, the possibility of their occurrence should be considered in patients who are sensitive to corticosteroid effects or when the usual doses of the drug are exceeded.
Patients with severe allergies should be instructed to avoid exposure to allergens during treatment with intranasal fluticasone propionate to prevent occurrence of severe allergic symptoms in the eyes and/or lower respiratory tract.
Use with caution in patients with clinical tuberculosis or asymptomatic Mycobacterium tuberculosis infections of the respiratory tract, untreated fungal or bacterial infections, ocular herpes simplex, or untreated, systemic viral infections.
Nasal passages should be examined periodically for mucosal changes and for signs of candidiasis during long-term therapy with fluticasone propionate. If such infections occur, appropriate local treatment of the infection may be necessary and/or discontinuance of intranasal fluticasone propionate therapy may be required.
Patients who are taking immunosuppressant drugs while receiving corticosteroids have increased susceptibility to infections (e.g., chickenpox, measles) compared with healthy individuals. If exposure to varicella or measles occurs, administration of varicella zoster immune globulin (VZIG) or intramuscular immunoglobulin (IG), respectively, may be indicated. If varicella develops, treatment with an antiviral agent (e.g., Acyclovir) may be considered.
Use in Children: The safety and efficacy of fluticasone propionate in children younger than 4 years old have not been established.
Use in Elderly: Adverse effects reported in elderly patients were similar to those reported by younger patients.
Avoid higher than recommended doses of fluticasone propionate nasal spray since hypercorticism and suppression of the hypothalamic-pituitary-adrenal (HPA) axis function may occur.
Patients who have received systemic corticosteroids for prolonged periods and transferred to topical corticosteroids should be monitored carefully since corticosteroid withdrawal symptoms (e.g., joint pain, muscular pain, lassitude, depression), acute adrenal insufficiency, or severe symptomatic exacerbation of asthma or other clinical conditions may occur.
Concomitant use of intranasal corticosteroids with other inhaled steroids may increase the risk of manifestations of hypercorticism and/or suppression of HPA axis function.
Although there have been no reports of manifestations of Cushing's syndrome (e.g., hypertension, glucose intolerance, cushingoid features) associated with intranasal fluticasone propionate therapy, the possibility of their occurrence should be considered in patients who are sensitive to corticosteroid effects or when the usual doses of the drug are exceeded.
Patients with severe allergies should be instructed to avoid exposure to allergens during treatment with intranasal fluticasone propionate to prevent occurrence of severe allergic symptoms in the eyes and/or lower respiratory tract.
Use with caution in patients with clinical tuberculosis or asymptomatic Mycobacterium tuberculosis infections of the respiratory tract, untreated fungal or bacterial infections, ocular herpes simplex, or untreated, systemic viral infections.
Nasal passages should be examined periodically for mucosal changes and for signs of candidiasis during long-term therapy with fluticasone propionate. If such infections occur, appropriate local treatment of the infection may be necessary and/or discontinuance of intranasal fluticasone propionate therapy may be required.
Patients who are taking immunosuppressant drugs while receiving corticosteroids have increased susceptibility to infections (e.g., chickenpox, measles) compared with healthy individuals. If exposure to varicella or measles occurs, administration of varicella zoster immune globulin (VZIG) or intramuscular immunoglobulin (IG), respectively, may be indicated. If varicella develops, treatment with an antiviral agent (e.g., Acyclovir) may be considered.
Use in Children: The safety and efficacy of fluticasone propionate in children younger than 4 years old have not been established.
Use in Elderly: Adverse effects reported in elderly patients were similar to those reported by younger patients.
Use In Pregnancy & Lactation
Pregnancy: The safe use of the product during pregnancy has not been established. Therefore, fluticasone propionate should be used in pregnancy only if the potential benefit justifies the potential risk to the fetus.
Lactation: It is not known if fluticasone propionate is excreted in breast milk. Therefore, do not administer to breastfeeding women unless, in the opinion of a physician, the potential benefits of the drug justify the possible risk to the baby.
Lactation: It is not known if fluticasone propionate is excreted in breast milk. Therefore, do not administer to breastfeeding women unless, in the opinion of a physician, the potential benefits of the drug justify the possible risk to the baby.
Adverse Reactions
General: Immediate hypersensitivity reactions including angioedema, rash, edema of the face and tongue, pruritus, urticaria, bronchospasm, wheezing, contact dermatitis, dyspnea, and anaphylaxis/anaphylactoid reactions have been reported with intranasal administration during post marketing studies.
Nasopharyngeal or Respiratory Effects: Epistaxis, nasal burning/irritation, pharyngitis, cough, asthma symptoms, nasal secretions containing blood, nasal discharge, bronchitis, sneezing, rhinorrhea, sinusitis, sore throat, throat irritation and dryness, hoarseness, voice changes, alteration or loss of sense of taste and/ or smell, nasal congestion, nasal dryness, nasal septum perforation, nasal septum crusting, nasal ulcer, and localized candidal infections of the nose and/or pharynx.
Gastrointestinal Effects: Nausea, vomiting, abdominal pain, diarrhea.
Ocular Effects: Dryness and irritation, conjunctivitis, blurred vision, glaucoma, increased intraocular pressure, and cataract.
Miscellaneous: Headache, dizziness, drowsiness, lethargy, fatigue or arthralgia, fever, flu-like symptoms, menstrual cramps, aches and pains, and cases of growth suppression have been reported.
Nasopharyngeal or Respiratory Effects: Epistaxis, nasal burning/irritation, pharyngitis, cough, asthma symptoms, nasal secretions containing blood, nasal discharge, bronchitis, sneezing, rhinorrhea, sinusitis, sore throat, throat irritation and dryness, hoarseness, voice changes, alteration or loss of sense of taste and/ or smell, nasal congestion, nasal dryness, nasal septum perforation, nasal septum crusting, nasal ulcer, and localized candidal infections of the nose and/or pharynx.
Gastrointestinal Effects: Nausea, vomiting, abdominal pain, diarrhea.
Ocular Effects: Dryness and irritation, conjunctivitis, blurred vision, glaucoma, increased intraocular pressure, and cataract.
Miscellaneous: Headache, dizziness, drowsiness, lethargy, fatigue or arthralgia, fever, flu-like symptoms, menstrual cramps, aches and pains, and cases of growth suppression have been reported.
Drug Interactions
Concomitant use with other inhaled or systemic corticosteroids may increase the risk of hypercorticism and/or suppression of HPA axis function.
Since fluticasone propionate is metabolized in the liver by the cytochrome P-450 (CYP) 3A4 isoenzyme, concomitant use of drugs that affect CYP hepatic microsomal enzymes may alter fluticasone's metabolism. Concomitant use of intranasal fluticasone propionate (200 mcg once daily) and ritonavir (100 mcg twice daily) may increase peak plasma concentrations and area under the plasma concentration-time curve (AUC) of fluticasone, resulting in decreased plasma cortisol AUC. During postmarketing experience, Cushing syndrome and adrenal suppression have been reported in patients receiving concomitant therapy of fluticasone propionate and ritonavir. Thus, concomitant use of these drugs is not recommended unless the potential benefit justifies the risk of systemic corticosteroid adverse effects.
Concurrent administration with ketoconazole may increase plasma fluticasone concentrations, reduce plasma cortisol AUC, and no effect on urinary excretion of cortisol.
Exercise caution when fluticasone is co-administered with other potent CYP3A4 inhibitors.
Since fluticasone propionate is metabolized in the liver by the cytochrome P-450 (CYP) 3A4 isoenzyme, concomitant use of drugs that affect CYP hepatic microsomal enzymes may alter fluticasone's metabolism. Concomitant use of intranasal fluticasone propionate (200 mcg once daily) and ritonavir (100 mcg twice daily) may increase peak plasma concentrations and area under the plasma concentration-time curve (AUC) of fluticasone, resulting in decreased plasma cortisol AUC. During postmarketing experience, Cushing syndrome and adrenal suppression have been reported in patients receiving concomitant therapy of fluticasone propionate and ritonavir. Thus, concomitant use of these drugs is not recommended unless the potential benefit justifies the risk of systemic corticosteroid adverse effects.
Concurrent administration with ketoconazole may increase plasma fluticasone concentrations, reduce plasma cortisol AUC, and no effect on urinary excretion of cortisol.
Exercise caution when fluticasone is co-administered with other potent CYP3A4 inhibitors.
Caution For Usage
Directions for Use: Before using: 1. Shake the bottle vigorously and remove the dust cap.
2. Hold the device with the forefinger and middle finger on either side of the nozzle and the thumb underneath the bottle.
3. Before initial use or if the product has not been used for several days, test the spray. With the nozzle pointing away from the body, press the nasal applicator several times until a fine mist comes out from the container.
Using the Spray: 4. Gently blow the nose to clear the nostril.
5. Close one nostril. Tilt the head slightly forward, keep the container upright, and carefully insert the nasal applicator into the open nostril.
6. Breathe in through the nose, and while breathing in press the while collar firmly down once to release a spray. Avoid spraying in eyes.
7. Breathe out through the mouth.
8. If a second spray is required in that nostril, repeat steps 4 to 6.
9. Repeat steps 4 to 7 in the other nostril.
After Use: 10. Wipe the nasal applicator with a clean tissue and replace the dust cap.
11. Rinse the mouth with water after finishing taking a dose. Do not swallow.
Cleaning Instructions: The nasal spray should be cleaned in the following way at least once a week: 1. Remove the dust cap.
2. Push on the white collar upward gently to detach the nasal applicator from the valve.
3. Wash the applicator and dust cap in warm water. Shake off the excess water and allow to dry at room temperature. Avoid excessive heat.
4. Push the applicator back on top of the bottle and replace the nasal applicator.
If the nasal applicator becomes blocked, soak the nasal applicator in warm water. Rinse with cold water, dry, and replace the nasal applicator. Do not use a pin or other sharp object to clean/unblock the nasal applicator.
2. Hold the device with the forefinger and middle finger on either side of the nozzle and the thumb underneath the bottle.
3. Before initial use or if the product has not been used for several days, test the spray. With the nozzle pointing away from the body, press the nasal applicator several times until a fine mist comes out from the container.
Using the Spray: 4. Gently blow the nose to clear the nostril.
5. Close one nostril. Tilt the head slightly forward, keep the container upright, and carefully insert the nasal applicator into the open nostril.
6. Breathe in through the nose, and while breathing in press the while collar firmly down once to release a spray. Avoid spraying in eyes.
7. Breathe out through the mouth.
8. If a second spray is required in that nostril, repeat steps 4 to 6.
9. Repeat steps 4 to 7 in the other nostril.
After Use: 10. Wipe the nasal applicator with a clean tissue and replace the dust cap.
11. Rinse the mouth with water after finishing taking a dose. Do not swallow.
Cleaning Instructions: The nasal spray should be cleaned in the following way at least once a week: 1. Remove the dust cap.
2. Push on the white collar upward gently to detach the nasal applicator from the valve.
3. Wash the applicator and dust cap in warm water. Shake off the excess water and allow to dry at room temperature. Avoid excessive heat.
4. Push the applicator back on top of the bottle and replace the nasal applicator.
If the nasal applicator becomes blocked, soak the nasal applicator in warm water. Rinse with cold water, dry, and replace the nasal applicator. Do not use a pin or other sharp object to clean/unblock the nasal applicator.
Storage
Store at temperatures not exceeding 30°C.
Action
Pharmacology: Pharmacodynamics: Mechanism of Action: Fluticasone propionate is a topically active, synthetic, trifluorinated corticosteroid. It has a high affinity for glucocorticoid receptor with negligible activity at androsterone, progesterone, estrogen, or mineralocorticoid receptors.
It has anti-inflammatory and immunosuppressant activities after topical application to the nasal mucosa.
In patients with allergic rhinitis, the onset of symptomatic relief may occur within 12 to 48 hours after initiation of intranasal fluticasone propionate therapy in adults and within 36 hours in children; however, in most patients, up to 2 to 4 days are required for optimum effectiveness.
Pharmacokinetics: Fluticasone propionate is poorly absorbed from the respiratory and gastrointestinal tracts after nasal inhalation as an aqueous spray. The absolute systemic bioavailability of intranasal fluticasone propionate is less than 2%. Much of the intranasal dose of corticosteroids is swallowed and undergoes extensive first-pass metabolism in the liver.
Fluticasone propionate is approximately 91% bound to human plasma proteins.
Fluticasone propionate is rapidly metabolized in the liver by the cytochrome P-450 isoenzyme CYP3A4. The main metabolic product is the 17β-carboxylic acid derivative, which is produced by esterase-catalyzed hydrolysis and has no significant glucocorticoid or anti-inflammatory activity. This is then largely excreted in feces, with less than 5% being excreted in urine.
It has anti-inflammatory and immunosuppressant activities after topical application to the nasal mucosa.
In patients with allergic rhinitis, the onset of symptomatic relief may occur within 12 to 48 hours after initiation of intranasal fluticasone propionate therapy in adults and within 36 hours in children; however, in most patients, up to 2 to 4 days are required for optimum effectiveness.
Pharmacokinetics: Fluticasone propionate is poorly absorbed from the respiratory and gastrointestinal tracts after nasal inhalation as an aqueous spray. The absolute systemic bioavailability of intranasal fluticasone propionate is less than 2%. Much of the intranasal dose of corticosteroids is swallowed and undergoes extensive first-pass metabolism in the liver.
Fluticasone propionate is approximately 91% bound to human plasma proteins.
Fluticasone propionate is rapidly metabolized in the liver by the cytochrome P-450 isoenzyme CYP3A4. The main metabolic product is the 17β-carboxylic acid derivative, which is produced by esterase-catalyzed hydrolysis and has no significant glucocorticoid or anti-inflammatory activity. This is then largely excreted in feces, with less than 5% being excreted in urine.
MedsGo Class
Nasal Decongestants & Other Nasal Preparations
Features
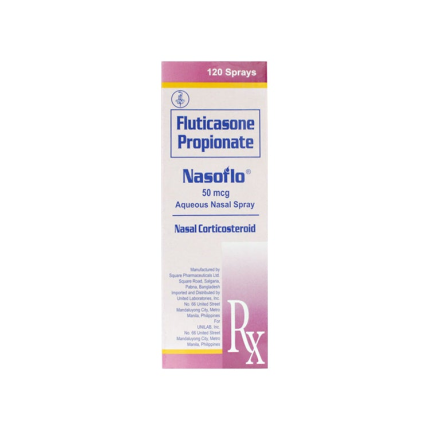
Dosage
50mcg
Ingredients
- Fluticasone
Packaging
Nasal Spray 120 sprays
Generic Name
Fluticasone Propionate
Registration Number
DR-XY34848
Classification
Prescription Drug (RX)
Reviews
No reviews found
Pharmacist answers to questions about NASOFLO Fluticasone Propionate 50mcg Nasal Spray 120 sprays
Questions