All variations
Indications / Uses
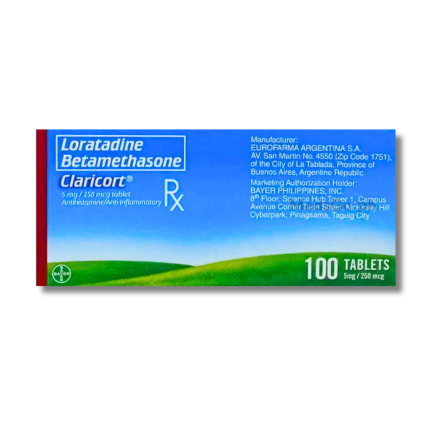
CLARICORT Loratadine / Betamethasone 5mg / 250mcg is used for the relief of inflammatory and pruritic manifestations of corticosteroid-responsive dermatoses when complicated by secondary infection caused by organisms susceptible to the components of the preparation or when the possibility of such infection is suspected. It is effective in treating respiratory and dermatological allergies such as allergic rhinitis and atopic dermatitis. This combination provides both antihistaminic and anti-inflammatory actions to manage complex allergic conditions efficiently.
Formulation / Ingredients
CLARICORT Loratadine / Betamethasone 5mg / 250mcg contains: Loratadine 5mg + Betamethasone 250mcg
Do I need prescription to buy CLARICORT Loratadine / Betamethasone 5mg / 250mcg?
Yes, you need a prescription. But if you don't have one, you can get a free teleconsultation from MedsGo Physician. Just make an order and our Physician will call you back.
Side Effects
CLARICORT Loratadine / Betamethasone 5mg / 250mcg common side effects include: fatigue, headache, somnolence, and dry mouth. Some users may also experience gastrointestinal disturbances such as gastritis or nausea. As it contains a corticosteroid, long-term use may lead to skin thinning, bruising, or fluid retention in sensitive individuals.
Directions and Dosage
- Adults and Adolescents (12+ years): 1 tablet twice daily. Do not exceed 2 tablets in 24 hours.
- Kids 6–12 years (Weight >30kg): 1 tablet twice daily.
- Kids 6–12 years (Weight <30kg): 1/2 tablet twice daily.
Not recommended for children under 6 years of age. Treatment should be limited to the shortest duration necessary to control symptoms, typically not exceeding 7 to 10 days unless specified otherwise.
Contraindications
Avoid use in individuals with systemic fungal infections or those who have shown hypersensitivity to any of the components. It is also contraindicated for patients with active tuberculosis or certain viral skin infections like herpes simplex or varicella.
Special Precautions
- Use with caution in patients with hepatic or renal insufficiency as dosage adjustments may be required.
- Monitoring is necessary for those with glaucoma, gastric ulcers, or hypertension due to the steroid component.
- Discontinue use if irritation or sensitization develops during the course of treatment.
Is it safe to take it with other medications?
Concurrent use with ketoconazole, erythromycin, or cimetidine may increase the plasma concentration of the antihistamine component. Certain drugs like phenobarbital may decrease the effectiveness of the corticosteroid.
How should I store it?
Store in a cool, dry place at temperatures not exceeding 30°C. Keep the container tightly closed and protect it from excessive light.
Used For
- Allergy and Inflammation
Age
- 6 years & up
Features
- Betamethasone
- Loratadine
Reviews
No reviews found
Pharmacist answers to questions about CLARICORT Loratadine / Betamethasone 5mg / 250mcg - 1 Tablet