Free delivery nationwide for orders above ₱800
+63(998)858-3957 Mon-Fr 9a.m.-6p.m.
+63(906)084-8874 Mon-Fr 9a.m.-6p.m.
Email contact@medsgo.ph
Address
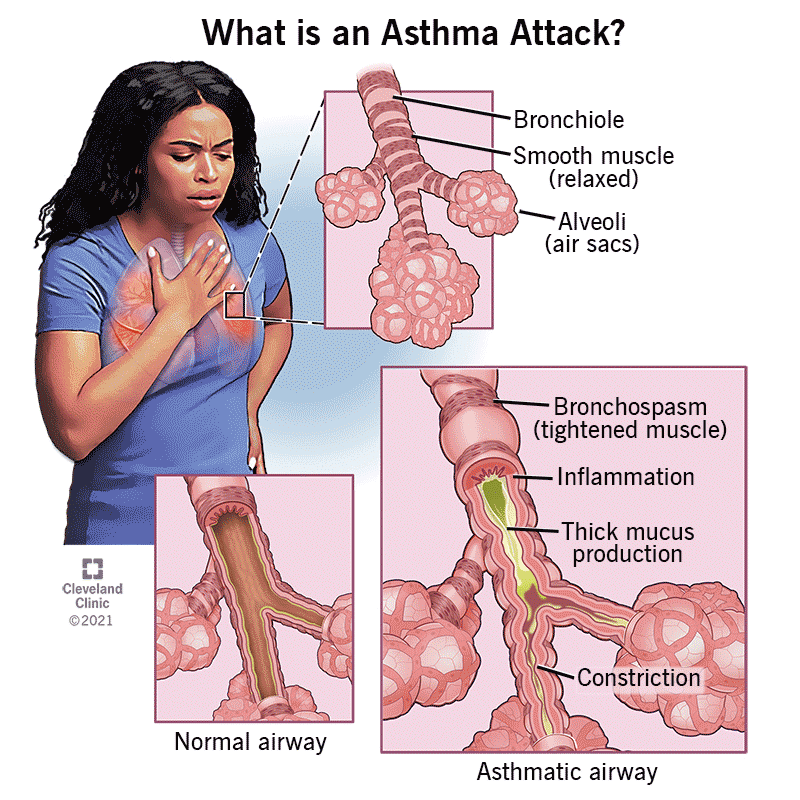
Understanding Asthma

Understanding Asthma: A Practical Guide for Patients and Caregivers
(https://my.clevelandclinic.org...)
Asthma is a long-term respiratory condition that affects how air moves in and out of the lungs. Because asthma symptoms and airflow limitation can vary over time, some days feel completely normal while other days can be more challenging (Nissly, 2022). When asthma is well controlled, people can live full, active lives with minimal symptoms. When asthma is uncontrolled, it can disrupt sleep, work, school, exercise, and overall quality of life (Global Initiative for Asthma [GINA], 2025; National Heart, Lung, and Blood Institute [NHLBI], 2007; Bateman et al., 2007; GINA, 2024).
This blog brings together practical, guideline-based steps patients and caregivers can use to stay in control.
What are the goals of asthma treatment?

(https://www.medkart.in/blog/as...)
Asthma care is built around two big goals: controlling symptoms now and reducing risk over time (GINA, 2024). Put simply, asthma treatment aims to:
- Control daily symptoms like coughing, wheezing, chest tightness, and shortness of breath
- Prevent asthma attacks (exacerbations) that may need urgent care or hospitalization
- Protect lung function over time
- Minimize medication-related side effects
These goals are consistently emphasized across clinical guidance, with the expectation that well-managed asthma allows people to sleep through the night, exercise, work, and participate in daily activities without limitations (GINA, 2025; NHLBI, 2007; NHLBI, 2020).
Asthma management is a team effort (and it works best that way)
Asthma care is most effective when patients and healthcare providers work collaboratively (GINA, 2025). Asthma management relies on four essential pillars:
- Patient education
- Trigger identification and avoidance
- Regular monitoring of symptoms and lung function
- Appropriate and consistent use of medications
Together, these pillars support good symptom control and lower future exacerbation risk (GINA, 2025; NHLBI, 2007; Mammen & McGovern, 2021; GINA, 2024).
Why patient education matters (more than people realize)

Asthma is largely managed outside the clinic, so education is a cornerstone of effective care (GINA, 2025). Strong education helps patients recognize symptoms early, identify triggers, and understand how to use medications correctly.
Structured asthma education typically covers:
- Common symptoms and early warning signs
- Personal triggers that worsen symptoms
- The difference between quick-relief and controller medications
- Correct inhaler technique
- How to follow an asthma action plan
Evidence links education and self-management support with fewer exacerbations, fewer hospitalizations/readmissions, and better quality of life (Gibson et al., 2000; Castro et al., 2003; Maricoto et al., 2016).
Using inhalers the right way: small mistakes, big impact

(https://www.who.int/news-room/...)
Inhaled medicines only work well when the device is used correctly—and incorrect technique is common (GINA, 2025; NHLBI, 2007). Large proportions of patients commit errors that reduce how much medicine reaches the lungs (Maricoto et al., 2016; UMass ScholarWorks, 2025).
Practical steps providers are encouraged to do include:
- Demonstrate the correct technique
- Watch the patient do it (teach-back/return demonstration) and give feedback
- Recommend spacers when appropriate
- Minimize the number of different inhaler devices when possible
Routine technique checks during follow-up are emphasized as a meaningful way to improve outcomes (GINA, 2025; Frontiers in Pharmacology, 2025; UMass ScholarWorks, 2025).
The asthma action plan: your “at-home playbook”
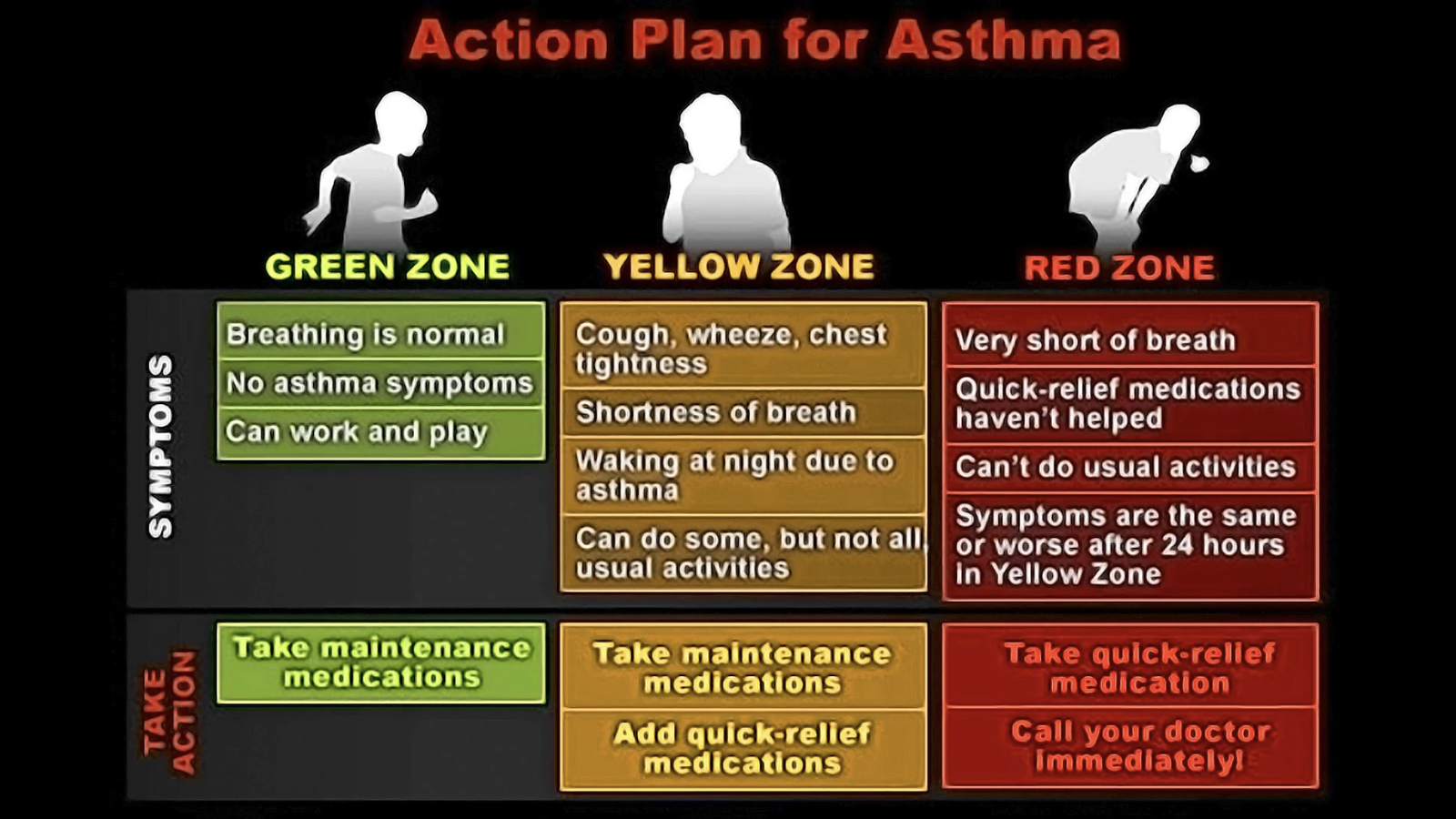
(https://storymd.com/journal/m8...)
An asthma action plan is a written, personalized guide that helps patients manage asthma at home. It typically includes:
- What medicines to take daily
- How to recognize worsening symptoms
- How to adjust treatment during flare-ups
- When to seek urgent care
Action plans are described as supporting self-management and helping reduce emergency visits, hospitalizations, and severe outcomes (NHLBI, 2007; NHLBI, 2020; GINA, 2024; GINA, 2025). They’re also commonly required by schools and childcare facilities (NHLBI, 2007; GINA, 2025).
Identifying and managing triggers
Asthma symptoms can worsen after exposure to triggers. Common triggers include:
- Allergens (dust mites, pollen, pets, mold) (GINA, 2025)
- Irritants (tobacco smoke, pollution, strong odors) (GINA, 2024; GINA, 2025)
- Respiratory infections (GINA, 2025; Nissly, 2022)
- Exercise (GINA, 2025; Nissly, 2022)
- Stress or hormonal changes (GINA, 2025; Nissly, 2022)
Identifying personal triggers helps patients reduce exposure when possible and adjust therapy when avoidance isn’t feasible, improving asthma control (GINA, 2025).
Vaccinations and infection prevention
Respiratory infections are highlighted as a major trigger for asthma flare-ups (CDC, 2022; GINA, 2025). Staying up to date on recommended vaccines can help you avoid this, including:
- Influenza
- Pneumococcal vaccines
- COVID-19 vaccines
- Pertussis
- RSV (when eligible)
Continuing prescribed asthma medications during mild respiratory infections is also noted as helpful in preventing severe exacerbations (CDC, 2022; GINA, 2025).
How asthma is assessed (and why objective testing matters)
Asthma assessment typically includes:
- Reviewing symptoms over recent weeks
- Checking how often quick-relief inhalers are used
- Evaluating activity limitations
- Measuring lung function when possible
Spirometry is emphasized as the preferred method for monitoring lung function in older children and adults (NHLBI, 2007; GINA, 2025). Home monitoring may include peak flow monitoring to detect early deterioration (NHLBI, 2007; NHLBI, 2020; GINA, 2025).
Asthma severity vs asthma control (not the same thing)
There are two important concepts:
- Asthma severity: the level of treatment needed to achieve control
- Asthma control: how well symptoms and risks are currently managed
A key takeaway is that even people with infrequent symptoms can still be at risk of severe exacerbations, which is why modern guidance emphasizes ongoing control rather than relying on labels alone (GINA, 2025; Reddel et al., 2009; Bateman et al., 2007; GINA, 2024).
Asthma medicines: relievers, controllers, and advanced options

(https://aafa.org/asthma/asthma...)
Asthma medicines are generally grouped into:
Reliever (rescue) medications
These provide rapid symptom relief, including:
- Short-acting beta-agonists (e.g., albuterol)
- Combination inhalers containing fast-acting bronchodilators and low-dose inhaled corticosteroids
(GINA, 2025; NHLBI, 2007)
Examples include:
Modern guidance (Track 1) prefers as-needed low-dose ICS-formoterol as a reliever approach in that framework (GINA, 2024; Mammen & McGovern, 2021).
Controller medications
These reduce airway inflammation and prevent symptoms over time, including:
- Inhaled corticosteroids (ICS)
- ICS + long-acting beta-agonist combinations
- Leukotriene receptor antagonists
- Biologic therapies for severe asthma
(GINA, 2025; NHLBI, 2007; Nissly, 2022)
Examples include:
Most patients with persistent asthma benefit from daily controller therapy to lower exacerbation risk (GINA, 2025; NHLBI, 2007).
Why regular follow-up is essential
Asthma changes over time, so follow-up visits matter. Routine follow-up (often every 1 to 6 months) is essential as an opportunity to:
- Assess control
- Review inhaler technique
- Adjust medications
- Address adherence and side effects
- Revisit triggers and lifestyle factors
(GINA, 2025)
Adjusting treatment over time: step up, step down
A stepwise approach is described consistently as:
- Step up treatment when asthma is uncontrolled
- Step down after sustained control, aiming for the lowest effective dose to minimize adverse effects
(GINA, 2025; NHLBI, 2007; NHLBI, 2020; GINA, 2024)
When to see a specialist
Referral to a pulmonologist or allergist may be needed when asthma is difficult to control, the diagnosis is uncertain, severe attacks occur, or high-dose/advanced therapies (including biologics) are being considered (Chung et al., 2014; Holguin et al., 2020; NHLBI, 2020; Practice Nurse, 2025).
Living well with asthma

(https://drrushidesai.com/asthm...)
Asthma can be challenging, but evidence emphasizes that most patients can achieve “well-controlled” asthma with the right education, support, and personalized plan (GINA, 2025; Bateman et al., 2007; GINA, 2024). Consistent medication use, early response to worsening symptoms, and open communication with the care team are recurring themes tied to long-term success (GINA, 2025).
Need Help Managing Your Asthma? MedsGo Offers FREE Teleconsultation
If you’re unsure which asthma medicine is right for you, or if you want guidance based on your symptoms, MedsGo offers FREE teleconsultation with licensed physicians. This service helps you get proper medical advice without leaving home—perfect for busy schedules, mobility concerns, or when you simply need quick, reliable guidance. You’ll receive professional assessment, safe dose recommendations, and help in choosing the right medications.
Book your free consult here: https://typeform.v.medsgo.ph/t...
References
Bateman, E. D., Hurd, S. S., Barnes, P. J., Bousquet, J., Drazen, J. M., FitzGerald, M., Gibson, P., Ohta, K., O’Byrne, P., Pedersen, S. E., Pizzichini, E., Sullivan, S. D., Wenzel, S. E., & Zar, H. J. (2007). Global strategy for asthma management and prevention: GINA executive summary. European Respiratory Journal, 31(1), 143–178. https://doi.org/10.1183/090319...
Castro, M., Zimmermann, N. A., Crocker, S., et al. (2003). Asthma intervention program prevents readmissions in high healthcare users. American Journal of Respiratory and Critical Care Medicine, 168(9), 1095–1099.
Centers for Disease Control and Prevention. (2022). Underlying medical conditions associated with high risk for severe COVID-19. https://www.cdc.gov/coronaviru...
Chung, K. F., Wenzel, S. E., Brozek, J. L., et al. (2014). International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. European Respiratory Journal, 43(2), 343–373.
Frontiers in Pharmacology. (2025). Effective inhaler technique education is achievable – Assessment and comparison of five inhaler devices errors. Frontiers in Pharmacology, 16. https://www.frontiersin.org/jo...
Gibson, P. G., Coughlan, J., Wilson, A. J., et al. (2000). Self-management education and regular practitioner review for adults with asthma. Cochrane Database of Systematic Reviews, CD001117.
Global Initiative for Asthma. (2024). Update on asthma management guidelines. https://pmc.ncbi.nlm.nih.gov/a...
Global Initiative for Asthma. (2025). Global strategy for asthma management and prevention. https://ginasthma.org
Holguin, F., Cardet, J. C., Chung, K. F., et al. (2020). Management of severe asthma: A European Respiratory Society/American Thoracic Society guideline. European Respiratory Journal, 55(1), 1900588.
Mammen, J. R., & McGovern, C. M. (2021). Summary of the 2020 focused updates to U.S. asthma management guidelines: What has changed and what hasn’t? Journal of the American Association of Nurse Practitioners, 34(2), 238–241. https://doi.org/10.1097/jxx.00...
Maricoto, T., Madanelo, S., Rodrigues, L., Teixeira, G., Valente, C., Andrade, L., & Saraiva, A. (2016). Educational interventions to improve inhaler techniques and their impact on asthma and COPD control: A pilot effectiveness-implementation trial. Jornal Brasileiro de Pneumologia, 42(6), 440–443. https://doi.org/10.1590/s1806-...
National Heart, Lung, and Blood Institute. (2007). Expert panel report 3: Guidelines for the diagnosis and management of asthma. https://www.nhlbi.nih.gov
National Heart, Lung, and Blood Institute. (2020). Asthma Care Quick Reference. https://www.nhlbi.nih.gov/file...
Nissly, T. (2022). Asthma management: How the guidelines compare. The Journal of Family Practice, 71(1). https://doi.org/10.12788/jfp.0...
Practice Nurse. (2025). The new asthma guidelines in real world clinical practice. https://practicenurse.co.uk/ar...
Reddel, H. K., Taylor, D. R., Bateman, E. D., et al. (2009). Asthma control and exacerbations: Standardizing endpoints for clinical asthma trials and clinical practice. American Journal of Respiratory and Critical Care Medicine, 180(1), 59–99.
UMass ScholarWorks. (2025). Increasing knowledge of inhaler technique in adult asthma and COPD patients. https://scholarworks.umass.edu...
No posts found
Write a review- Mandaluyong, Unit B, LN Bldg., 738 Shaw Blvd., Greenfield District, Highway Hills
- +63(998)858-3957
- +63(906)084-8874
- Mon-Sun 9.00 - 18.00
- contact@medsgo.ph
- View on map
© 2023 - 2026 MedsGo Pharmacy Chain. FDA License Number CDRR-NCR-DS-573920
