All variations
Indications / Uses
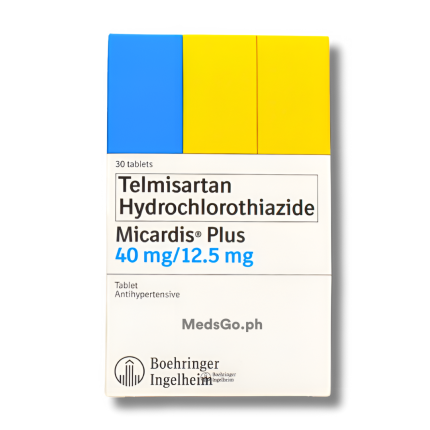
MICARDIS PLUS Telmisartan / Hydrochlorothiazide 40 / 12.5 is used for the management of essential hypertension (high blood pressure) when pressure control is not adequately achieved with either telmisartan or hydrochlorothiazide alone. The combination of its two active components provides a synergistic blood pressure-lowering effect. Telmisartan acts by blocking a substance that causes blood vessels to narrow, while hydrochlorothiazide works as a diuretic to reduce excess body fluid. This dual mechanism helps to achieve effective blood pressure control, which is crucial for reducing the long-term risk of serious health issues.
Formulation / Ingredients
MICARDIS PLUS Telmisartan / Hydrochlorothiazide 40 / 12.5 contains: Telmisartan 40mg + Hydrochlorothiazide 12.5mg
Do I need prescription to buy MICARDIS PLUS Telmisartan / Hydrochlorothiazide 40 / 12.5?
Yes, you need a prescription. But if you don't have one, you can get a free teleconsultation from MedsGo Physician. Just make an order and our Physician will call you back.
Side Effects
MICARDIS PLUS Telmisartan / Hydrochlorothiazide 40 / 12.5 common side effects include: dizziness, headache, and a general feeling of tiredness or fatigue. Gastrointestinal issues such as nausea and diarrhea may also occur as the body adjusts to the preparation. Due to the diuretic component, changes in body fluid and electrolyte levels can lead to symptoms like muscle cramps or weakness, and it may also cause mild hypotension. If any unusual symptoms are observed, a medical evaluation is advised.
Directions and Dosage
- Dosage for Adults (18+ years): 1 tablet daily.
The maximum daily dosage should not exceed 1 tablet of this strength. Not recommended for individuals under 18 years of age due to lack of established safety and effectiveness in this population.
Contraindications
Avoid use if there is severe impairment of liver or kidney function, including issues with bile flow from the gallbladder. It is also contraindicated in individuals with treatment-resistant electrolyte imbalances, such as low blood potassium or sodium, or very high blood calcium levels. Should not be used in those with a history of gout or a known sensitivity to any component of the tablet.
Use in Pregnancy and Lactation
Use is strictly avoided during pregnancy as it may cause harm to the developing fetus. It should also be avoided while breastfeeding, as it is unknown if the active components pass into the milk and could potentially affect the infant.
Special Precautions
- Close monitoring is necessary for individuals with pre-existing heart or kidney issues, including reduced blood volume due to severe vomiting or diarrhea.
- Use with caution in those with systemic lupus erythematosus or a history of primary hyperaldosteronism.
- Periodic evaluation of blood electrolyte levels may be required for those on a low-salt diet or who may be prone to imbalance.
- Caution is advised in individuals with a history of non-melanoma skin cancer or certain eye problems.
Is it safe to take it with other medications?
Combining this product with other blood pressure-lowering agents may lead to excessive reduction in pressure. Particular care is needed when taken with potassium supplements, potassium-sparing agents, or certain non-steroidal anti-inflammatory preparations, as this can affect kidney function and electrolyte balance. The combined administration may also increase the concentration of lithium in the body.
How should I store it?
Keep the tablets in their original packaging to protect them from light and moisture. Store at a temperature not exceeding 30°C and ensure the container is tightly closed.
Used For
- High Blood Pressure
Age
- Adults (18+ years)
Features
- Hydrochlorothiazide
- Telmisartan
Reviews
No reviews found
Product Questions